CPI
Center for Program Integrity
Protecting the Medicare & Medicaid Programs from Fraud, Waste, and Abuse
The Healthcare Fraud Prevention Partnership continues to grow, with more than 300 partners sharing the goal of eliminating healthcare fraud, waste, and abuse.
Review Choice Demonstration for Home Health Services. Learn more about our newly released Home Health RCD stats.
The National Correct Coding Initiative provides resources for Medicare and Medicaid providers to ensure proper claim coding.
Learn about the Open Payments program, promoting transparency of the $12.59 billion in payments made to providers and hospitals in 2022.
Who We Are
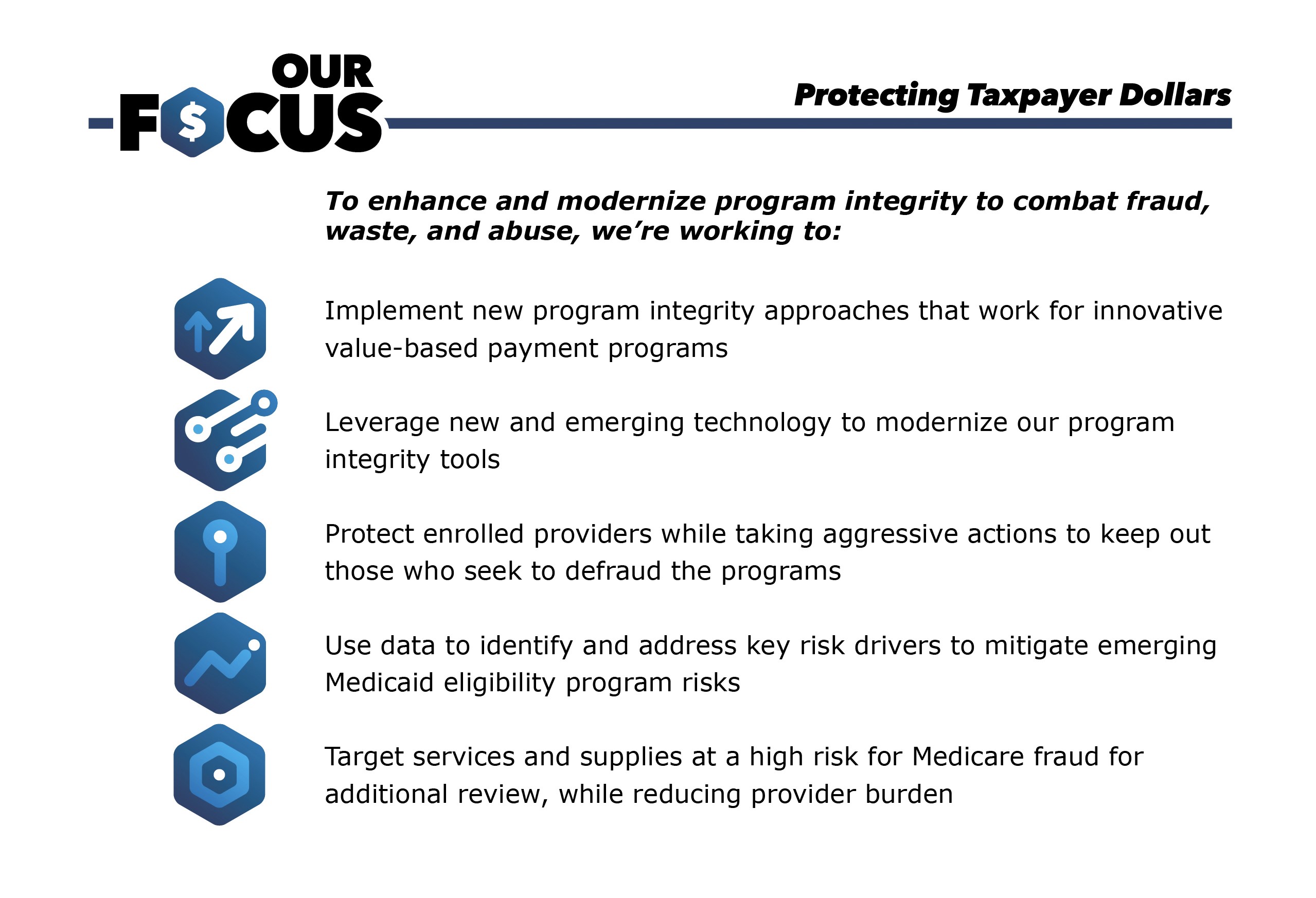
At the Center for Program Integrity (CPI), our mission is to detect and combat fraud, waste and abuse of the Medicare and Medicaid programs. We do this by making sure CMS is paying the right provider the right amount for services covered under our programs. We work with providers, states, and other stakeholders to support proper enrollment and accurate billing practices. Our work focuses on protecting patients while also minimizing unnecessary burden on providers.
Meet CPI’s Leadership Team and view our Functional Statement.
What We Do
CPI builds systems and manages programs to enroll providers in the Medicare and Medicaid programs.
Using predictive analytics, we identify and seek to prevent fraud, waste and abuse. See an example of how data is used to understand the health care landscape with the Market Saturation and Utilization map.
CPI oversees medical reviews and audits to safeguard the Medicare and Medicaid programs from fraud, waste and abuse.
CPI offers support and venues for states to collaborate and share best fraud-fighting practices, making the Medicaid program stronger and protecting the care of states’ Medicaid populations.
Shortcuts
Stay Up to Date with CPI
Connect with CPI as we host or attend various events throughout the year, join our mailing list to stay informed on Program Integrity news, or find the most appropriate vehicle to report suspected fraud, waste, or abuse.