Lesson 1: Introduction & Learning
Objectives
This lesson describes fraud, waste, and
abuse (FWA) and the laws that prohibit it. It should take you about 10 minutes
to complete.
After completing this lesson, you should
be able to:
* Recognize FWA in the Medicare Program
* Identify major FWA laws and regulations
* Recognize potential consequences and violation penalties

Fraud
Fraud is knowingly submitting, or
causing to be submitted, false claims or making misrepresentations of fact to
get a federal health care payment when no entitlement would otherwise exist.
Knowingly soliciting, getting, offering, or paying remuneration (for example,
kickbacks, bribes, or rebates) to induce or reward referrals for items or
services reimbursed by federal health care programs. Making prohibited
referrals for certain designated health services is another example.
Fraud requires intent to get payment and knowledge the actions are
wrong.

Fraud (continued)
The Criminal Health Care Fraud Statute
(18 United States Code (USC) 1347) makes it a criminal offense to knowingly and
willfully execute a scheme to defraud a health care benefit program. Health
care fraud is punishable by imprisonment up to 10 years. It’s also subject to
criminal fines up to $250,000. The statute prohibits knowingly and willfully
executing, or attempting to execute, a scheme or lie connected to delivering or
paying for health care benefits, items, or services to either:
* Defraud any health care benefit
program
* Get (by means of false or fraudulent pretenses, representations, or promises)
money or property owned by, or controlled by, any health care benefit program
Example: Several doctors and
medical clinics conspire in a coordinated scheme to defraud the Medicare
Program by submitting medically unnecessary power wheelchair claims.
Penalties: Penalties for
violating the Criminal Health Care Fraud Statute may include fines, imprisonment,
or both.
Waste & Abuse
Waste describes practices that, directly or
indirectly, result in unnecessary Medicare Program costs, like overusing
services. Waste is generally not considered to be criminally negligent but
rather the misuse of resources.
Abuse describes practices that, directly or
indirectly, result in unnecessary Medicare Program costs. Abuse includes any
practice that doesn’t provide patients with medically necessary services or
meet professionally recognized standards of care.
Section 20 of Medicare
Managed Care Manual, Chapter 21 and Prescription Drug Benefit Manual, Chapter 9 have fraud, waste, and abuse definitions.
Fraud, Waste, & Abuse Examples
Medicare fraud examples:
* Knowingly billing for services of
higher complexity than services actually provided or
documented in patient medical records
* Knowingly billing for services or supplies not provided, including falsifying
records to show item delivery
* Knowingly ordering medically unnecessary patient items or services
* Paying for federal health care program patient referrals
* Billing Medicare for appointments patients don’t keep
Medicare waste examples:
* Conducting excessive office visits or
writing excessive prescriptions
* Prescribing more medications than necessary for treating a specific condition
* Ordering excessive lab tests
Medicare abuse examples:
* Billing unnecessary medical services
* Charging excessively for services or supplies
* Misusing codes on a claim, like upcoding (assigning an inaccurate medical procedure
or treatment billing code to increase payment) or unbundling codes
Fraud, Waste, & Abuse Differences
There are differences between fraud,
waste, and abuse. One of the primary differences is intent and knowledge. Fraud
requires intent to get payment and knowledge the actions are wrong. Waste and
abuse may involve getting an improper payment or creating unnecessary Medicare
Program costs but don’t require the same intent and knowledge.

Understanding Fraud, Waste, & Abuse
To detect FWA, you need to know the law.
The next pages provide high-level
information about these laws:
* Federal Civil False Claims Act (FCA)
* Criminal Health Care Fraud Statute
* Anti-Kickback Statute (AKS)
* Physician Self-Referral Law (Stark Statute)
* Civil Monetary Penalties Law (CMPL)
* Exclusion Statute
* Health Insurance Portability and Accountability Act (HIPAA)
For details about specific laws, review
the applicable statute and regulations.
Federal Civil False Claims Act
The civil False Claims Act (FCA) (31 USC
3729–3733) makes a person liable to pay damages to the government if they knowingly:
* Conspire to violate the FCA
* Carry out other acts to get government property by misrepresentation
* Conceal or improperly avoid or decrease an obligation to pay the government
* Make or use a false record or statement supporting a false claim
* Present a false claim for payment or approval
Additionally, under the criminal FCA (18
USC 287), individuals or entities may face criminal penalties, including fines,
imprisonment, or both for submitting false, fictitious, or fraudulent claims.
Examples:
A Florida Medicare Part C plan:
* Hired an outside company to review
medical records to find additional diagnosis codes it could submit to increase
CMS risk capitation payments
* Was informed by the outside company that certain diagnosis codes previously
submitted to Medicare were undocumented or unsupported
* Failed to report the unsupported diagnosis codes to Medicare
* Agreed to pay $22.6 million to settle FCA allegations
The owner-operator of a California
medical clinic:
* Used marketers to recruit individuals
for medically unnecessary office visits
* Promised free, medically unnecessary equipment or free food to entice
individuals
* Charged Medicare more than $1.7 million for the scheme
* Was sentenced to 37 months in prison
Damages & Penalties
Penalties for violating the civil FCA may include recovery of up to 3
times the amount of the government’s damages due to the false claims, plus
$11,000 per false claim filed.
Federal Civil False Claims Act
(continued)
Whistleblower: A person who exposes
information or activity that’s deemed illegal, dishonest, or violates
professional or clinical standards
Protected: A person who reports false claims or brings legal actions to recover
money paid on false claims is protected from retaliation
Rewarded: A person who brings a successful whistleblower lawsuit gets at
least 15%, but not more than 30%, of the money the
government collects
Criminal Health Care Fraud Statute
The Criminal Health Care Fraud Statute
(18 USC 1346–1349) states, “Whoever knowingly and willfully executes, or
attempts to execute, a scheme or artifice to defraud any health care benefit
program or obtain, by means of false or fraudulent pretenses, representations,
or promises, any of the money or property owned by, or under the custody or
control of, any health care benefit program … shall be fined under this title
or imprisoned not more than 10 years, or both.”
Conviction under the statute doesn’t
require proof the violator knew the law or had specific intent to violate it.
Examples:
A Pennsylvania pharmacist:
* Submitted Medicare Part D claims for
non-existent prescriptions and drugs not dispensed
* Pleaded guilty to health care fraud
* Got a 15-month prison sentence and was ordered to pay more than $166,000 in
restitution to the plan
The owner of multiple New York Durable
Medical Equipment (DME) companies:
* Falsely represented themselves as 1 of
a nonprofit health maintenance organization’s (that
administered a Medicare Advantage plan) authorized vendors
* Didn’t provide DME to any patients as claimed
* Submitted almost $1 million in false claims to the nonprofit; was paid
$300,000
* Pleaded guilty to 1 count of conspiracy to commit health care fraud
Criminal Health Care Fraud Statute
(continued)
Persons who knowingly make a false claim
may be subject to:
* Criminal fines up to $250,000
* Imprisonment for up to 20 years
If the violations resulted in death, the
individual may be imprisoned for any term of years or for life.
18 USC 1347 has more information.
Anti-Kickback
Statute
The
Anti-Kickback Statute (AKS) (42 USC 1320a-7b(b)) makes it a crime to knowingly
and willfully offer, pay, solicit, or get any remuneration directly or indirectly
to induce or reward patient referrals or business generation involving any item
or service payable by a federal health care program. When a provider offers,
pays, solicits, or gets unlawful remuneration, they violate the AKS.
The
safe harbor regulations (42 CFR 1001.952) describe various payment and business
practices that, although they potentially implicate the AKS, aren’t treated as
AKS offenses if they meet certain regulatory requirements. Individuals and
entities remain responsible for complying with all other laws, regulations, and
guidance that apply to their businesses.
Comparison
of the Anti-Kickback Statute and Stark Law handout has more information.
Example:
A
physician operating a Rhode Island pain management practice:
*
Conspired to solicit and get kickbacks for prescribing a highly addictive
version of the opioid Fentanyl
* Reported patients had breakthrough cancer pain to secure insurance payments
* Got $188,000 in speaker fee kickbacks from the drug manufacturer
* Admitted the kickback scheme cost Medicare and other payers more than
$750,000
The
physician was required to pay more than $750,000 in restitution.
Damages
& Penalties
Violations
are punishable by:
*
A fine up to $25,000
* Imprisonment up to 5 years, or both
Section
1128B(b) of the Social Security Act has more information.
Physician
Self-Referral Law (Stark Law)
The
Physician Self-Referral Law (42 USC 1395nn), often called the Stark Law,
prohibits a physician from referring a patient to get designated health services
from a provider with whom a physician or a physician’s immediate family member
has a financial relationship, unless an exception applies.
Designated
health services:
*
Clinical lab services
* Physical therapy, occupational therapy, and outpatient speech-language
pathology services
* Radiology and other imaging services
* Radiation therapy services and supplies
* DME and supplies
* Parenteral and enteral nutrients, equipment, and supplies
* Prosthetics, orthotics, and supplies
* Home health services
* Outpatient prescription drugs
* Inpatient and outpatient hospital services
Damages
& Penalties
We
don’t pay Medicare claims tainted by an arrangement that doesn’t comply with
the Stark Statute. A penalty of appoximately $25,000
can be imposed for each service provided. There may also be a fine over
$160,000 for entering into an unlawful arrangement or scheme.
Physician
Self-Referral webpage and section 1877 of the
Social Security Act have more information.
Example:
A
California hospital was ordered to pay more than $3.2 million to settle Stark
Law violations for maintaining 97 financial relationships with physicians and
physician groups outside the fair market value standards or that were
improperly documented as exceptions.
Civil
Monetary Penalties Law
The
Civil Monetary Penalties Law (CMPL) (42 USC 1320a-7a) authorizes the Office of
Inspector General (OIG) to seek Civil Monetary Penalties (CMPs) and sometimes
exclusions for a variety of health care fraud violations. Violations that may
justify CMPs include:
*
Arranging for an excluded individual’s or entity’s services or items
* Failing to grant OIG timely records access
* Filing a claim you know or should know is for an item or service that wasn’t
provided as claimed or is false or fraudulent
* Filing a claim you know or should know is for an item or service for which we
won’t make payment
* Violating the AKS
* Violating Medicare assignment provisions
* Violating the Medicare physician agreement
* Providing false or misleading information expected to influence a discharge
decision
* Failing to provide an adequate medical screening exam for patients who
present to a hospital emergency department with an emergency medical condition
or in labor
* Making false statements or misrepresentations on applications or contracts to
participate in federal health care programs
Section
1128A(a) of the Social Security Act has more information.
Example:
A
California pharmacy and its owner agreed to pay over $1.3 million to settle
allegations they submitted unsubstantiated Medicare Part D claims for brand
name prescription drugs the pharmacy couldn’t have dispensed based on inventory
records.
Damages & Penalties
Penalties
and assessments vary
based on the type of violation. Penalties can be approximately $10,000–$50,000
per violation. CMPs may also include an assessment of up to 3 times the amount
claimed for each item or service, or up to 3 times the amount of remuneration
offered, paid, solicited, or received.

Exclusion Statute
The Exclusion Statute (42 USC 1320a-7) requires
the OIG exclude individuals and entities convicted of these offenses from
participating in all federal health care programs:
* Medicare or Medicaid fraud, as well as
other offenses related to delivering Medicare or Medicaid items or services
* Patient abuse or neglect
* Felony convictions for other health care-related fraud, theft, or other
financial misconduct
* Felony convictions for unlawful manufacture, distribution, prescribing, or
dispensing controlled substances
The OIG also maintains the List of
Excluded Individuals and Entities (LEIE) website.
The U.S. General Services Administration
(GSA) administers the Excluded Parties List System (EPLS), which enables
various federal agencies, including the OIG, to take debarment actions.
When looking for excluded individuals or
entities, check both the LEIE and the EPLS since the lists aren’t the same. 42
CFR 1001.1901 has more information.
Example:
A pharmaceutical company pleaded guilty
to 2 felony counts of criminal fraud for not filing required reports with the
FDA about oversized morphine sulfate tablets. The pharmaceutical firm executive
was excluded based on the company’s guilty plea. When the unconvicted
executive was excluded, there was evidence he was involved in misconduct
leading to the company’s conviction.

Health
Insurance Portability and Accountability Act
The
Health Insurance Portability and Accountability Act (HIPAA) created greater
access to health care insurance, strengthened health care data privacy protection,
and promoted health care industry standardization and efficiency.
HIPAA
safeguards deter unauthorized access to protected health care information. As
someone with access to protected health care information, you must comply with
HIPAA.
Example:
A
former hospital employee pleaded guilty to criminal HIPAA charges after getting
protected health information with the intent to use it for personal gain. He
was sentenced to 12 months and 1 day in prison.
Damages
& Penalties
Violations
may result in CMPs. In some cases, criminal penalties may apply.

Lesson 1 Summary
There are differences between fraud, waste,
and abuse (FWA). One of the primary differences is intent and knowledge.
Fraud is knowingly submitting, or
causing to be submitted, false claims or making misrepresentations of fact to
get a federal health care payment for which no entitlement would otherwise
exist.
Waste and abuse may involve getting an
improper payment but not the same intent and knowledge.
Laws and regulations exist that prohibit
FWA. Penalties for violating these laws include:
* Civil Monetary Penalties
* Civil prosecution
* Criminal conviction, fines, or both
* Exclusion from all federal health care program participation
* Imprisonment
* Loss of professional license
Review Questions
You reviewed the differences between
fraud, waste and abuse. The next pages ask review questions
to help reinforce this knowledge.
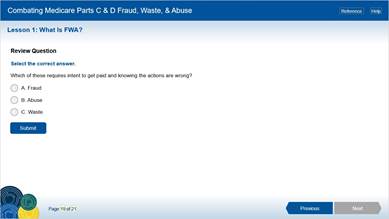
Review
Question
Select
the correct answer.
Which
of these requires intent to get paid and knowing the actions are wrong?
A. Fraud
B. Abuse
C. Waste

Review Question
Select the correct answer.
Which of these is NOT a potential
penalty for violating laws or regulations prohibiting fraud, waste, and abuse
(FWA)?
A.
Civil Monetary Penalties (CMPs)
B. Deportation
C. Exclusion from participation in all
federal health care programs
You’ve completed Lesson 1: What’s Fraud,
Waste, & Abuse?
Now that you’ve learned about FWA and
the laws and regulations prohibiting it, let’s look closer at your role in the
fight against FWA.
Select Continue to return to the Course
Menu. Then, select Lesson 2: Your Role in the Fight Against Fraud, Waste, &
Abuse.