Establishing the Framework for Health Equity at CMS
For far too long, health care disparities have persisted in the United States. In 1985, the landmark report, titled Report of the Secretary’s Task Force on Black and Minority Health (Heckler Report),[1] marked the first convening of a group of health experts by the U.S. government to conduct a comprehensive study of racial and ethnic minority health and elevate minority health to a national stage. It found persistent health disparities accounted for 60,000 excess deaths each year.[2] Despite progress, health disparities persist, rooted in centuries of structural and systemic barriers in the health care system, and across other systems, having direct impacts on a person’s health.
Fast forward to January 2021, President Biden issued Executive Order 13985, Advancing Racial Equity and Support for Underserved Communities Through the Federal Government,[3] and other executive orders focused on equity. For the first time in recent history, the Centers for Medicare & Medicaid Services (CMS), and all other federal agencies, are being charged with a whole-of-government approach to find out what more we can do across our work to identify, understand, and address structural, policy, and operational challenges and barriers to equity.
CMS defines health equity as the attainment of the highest level of health for all people, where everyone has a fair and just opportunity to attain their optimal health regardless of race, ethnicity, disability, sexual orientation, gender identity, socioeconomic status, geography, preferred language, or other circumstances.[4] CMS is working to advance health equity in three critical ways:
- Designing, implementing, and operationalizing policies and programs that support the health of all the people CMS serves.
- Eliminating avoidable differences in health outcomes experienced by people who are disadvantaged or underserved.
- Providing the care and support that our enrollees need to thrive.
CMS is the nation’s largest health insurer and has a critical role in driving improvements in health equity over the next decade. As CMS continues to lead the way to a more equitable health care system, we are taking another bold step in asserting our commitment to move our health care system from disparities to equity, through the release of the CMS Framework for Health Equity (Framework).
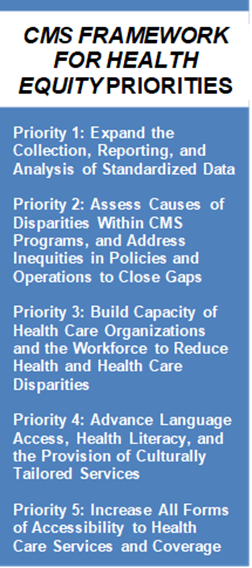
The Framework provides an integrated, action-oriented approach for CMS to advance health equity among members of communities who have been historically underserved or disadvantaged and for providers, plans, and other organizations serving such communities. Outlining five priority areas, this Framework updates the 2015 Medicare-focused CMS Equity Plan for Improving Quality in Medicare[5] with an enhanced and more comprehensive 10-year plan to further embed health equity across all CMS programs, including Medicare, Medicaid, the Children’s Health Insurance Program (CHIP), and the Marketplace.
The Framework reflects CMS’s commitment to health equity. In identifying advancing equity as the first pillar in the CMS Strategic Plan,[6] ,[7] Administrator Chiquita Brooks-LaSure has charged CMS to advance health equity across the CMS programs of Medicare, Medicaid and CHIP, and the Marketplace. As the major payor for the health care system, CMS can have large role in aligning equity with the systems of care and payment models. For example, Administrator Brooks-LaSure directed the Centers for Clinical Standards and Quality (CCSQ) to propose a “Birthing-Friendly” hospital designation that identifies hospitals that demonstrate a commitment to improving maternity care quality through their participation in quality improvement collaboratives and implementation of best practices that advance health care quality, safety, and equity for pregnant and postpartum parents. CMS is committed to taking an integrated, action-oriented approach to advance health equity.
Underlying this directive is the approach CMS will use to operationalize efforts to achieve health equity in its programs and policies. The Framework provides a strong foundation for our work as a leader and trusted partner dedicated to advancing health equity, expanding coverage, and improving health outcomes.
The Framework is based on a decade of evidence-based research and stakeholder input and direction. In particular, when we work to advance health equity, we focus on the needs and voices of members of racial and ethnic communities, people with disabilities, members of the lesbian, gay, bisexual, transgender, and queer community, individuals with limited English proficiency, members of rural communities, and others adversely affected by persistent poverty or inequality.
Without data, we cannot fully understand the disparities or know who is most impacted and where the gaps exist in quality, access, and outcomes, which is why expanding the collection, reporting, and analysis of standardized data is the first priority listed in the Framework. We are looking internally at expanding collection, reporting, and stratification of data across our programs, thinking about health equity-focused measures, working towards building health equity reporting metrics into our quality improvement programs, and working to increase the availability of, and access to, CMS data for researchers and our external partners.
The second priority of the Framework focuses on assessing causes of disparities within CMS programs and addressing inequities in policies and operations to close gaps. This reflects CMS’ focus on identifying and removing barriers our populations experience as they seek to access and use CMS-supported benefits, services, and coverage. We are working toward this priority through models and pilots where equity and disparity reduction are guiding principles and by focusing on responsive outreach and engagement with the communities we serve to understand barriers. We are also taking action to address barriers, which includes rolling back restrictive policies that inhibit access to coverage and care in Medicaid, implementing 12-month postpartum coverage in Medicaid, and increasing enrollment efforts in Marketplace plans among underrepresented communities.
The third priority focuses on building capacity of health care organizations and workforce to reduce disparities. Within this priority, we are continuously examining whether health care professionals and organizations have the tools they need to do their work in local communities. We are paying particular attention to understanding and meeting the needs of the whole health care team, including providers, plans, and other organizations that disproportionately serve underserved communities, to ensure CMS programs are structured in ways that allow these providers and networks to fully realize the intended benefits of these programs for all people CMS programs serve. For example, CMS is considering ways to encourage safety net provider participation in accountable care organizations and value-based care and ways to structure our programs to support providers in identifying and addressing social risk factors and social determinants of health as they provide care and coverage.
We cannot achieve health equity if people do not understand health coverage and health services. Priority four focuses on advancing language access, health literacy, and the provision of culturally tailored services. Here we focus on helping organizations — and CMS — implement the National Standards for Culturally and Linguistically Appropriate Services (CLAS).[8] We are working toward ensuring CMS materials are in multiple languages and at appropriate literacy levels and that navigators and certified application counselors are available to help consumers enroll in the right health care plans to meet their financial and health care needs. As we implement laws, such as the No Surprises Act,[9] we also seek to ensure that members of underserved communities are able to understand their rights and access protections related to surprise medical bills and unexpected health care costs.
Finally, with priority five, we are increasing all forms of accessibility to health care services and coverage so that all people with disabilities have improved access to quality health care coverage, services and supports, and benefits. In addition to working to support providers in delivering high quality care tailored to the needs of people with disabilities, we are also thinking about our health and safety standards through an accessibility lens. Of critical importance, we are working to promote broader coverage of services that address health-related social needs, such as nutrition supports, home modifications, wrap-around housing supports, and other services. These supports, as well as home health care and other home and community-based services, help older individuals and individuals with disabilities access the care and support they, their families, and caregivers need.
This Framework challenges CMS to incorporate advancing health equity as a foundational element across all our work, in every program, across every community. We are designing, implementing, and operationalizing policies and programs that support health for all the people served by our programs, eliminating avoidable differences in health outcomes experienced by people who are disadvantaged or underserved, and providing the care and support that our enrollees need to thrive.
CMS oversees the health coverage of more than 150 million people.[10] It is crucial for CMS to be bold and steadfast in its commitment to equity. As we move forward, our intent and unwavering commitment to advancing health equity will help support a health care system that benefits future generations.
CMS cannot do this alone. It is our collective responsibility to engage and be a part of advancing health equity. CMS will continue its partnership with our local communities, states, U.S. territories, tribal nations, providers, plans, quality improvement partners, and social service providers to work to achieve health equity. We need our communities, stakeholders, health care professionals, and each of you to stay involved, stay connected with us, and challenge yourself on how you can advance health equity in your own work. Together, we can help all people served by CMS achieve their highest level of health possible.
To find out more about the CMS Office of Minority Health, visit https://go.cms.gov/omh.
[3] https://www.whitehouse.gov/briefing-room/presidential-actions/2021/01/20/executive-order-advancing-racial-equity-and-support-for-underserved-communities-through-the-federal-government/
[4] https://www.cms.gov/pillar/health-equity
[5] https://www.cms.gov/about-cms/agency-information/omh/omh_dwnld-cms_equityplanformedicare_090615.pdf
[10] https://www.cms.gov/pillar/expand-access