On January 18, 2024, the Centers for Medicare & Medicaid Services (CMS) announced the Innovation in Behavioral Health (IBH) Model.
IBH is focused on improving quality of care and behavioral and physical health outcomes for Medicaid and Medicare populations with moderate to severe mental health conditions and substance use disorder (SUD). Medicare and Medicaid populations experience disproportionately high rates of mental health conditions and/or substance use disorders (SUD), and as a result are more likely to experience poor health outcomes and experiences, like frequent visits to the emergency department and hospitalizations, or premature death.
The IBH Model seeks to bridge the gap between behavioral and physical health; practice participants under the IBH Model will screen and assess patients for select health conditions, as well as mental health conditions and/or SUD, in community-based behavioral health practices. IBH is a state-based model, led by state Medicaid Agencies, with a goal of aligning payment between Medicaid and Medicare for integrated services.
CMS will release a Notice of Funding Opportunity (NOFO) in Spring 2024, and up to eight states will be selected to participate. The model will launch in Fall 2024 and run for eight years.
Model Overview
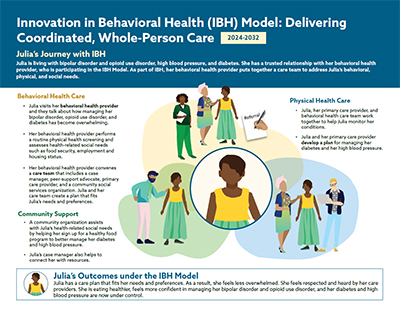
The Innovation in Behavioral Health (IBH) Model is designed to deliver person-centered, integrated care to Medicaid and Medicare populations with moderate to severe mental health conditions and/or substance use disorder (SUD). The practice participants in the IBH Model will be community-based behavioral health organizations and providers, including Community Mental Health Centers, opioid treatment programs, safety net providers, and public or private practices, where individuals can receive outpatient mental health and/or SUD services. These practice participants may include safety net providers who ensure that vulnerable populations are able to access care.
Practice participants will lead an interprofessional care team and be responsible for coordinating with other members of the care team to comprehensively address a patient’s care to include behavioral and physical health, and health-related social needs (HRSN) such as housing, food, and transportation.
The practice participants will conduct an initial screening and assessment, offer treatment or referrals to other care specialists and community-based resources, and monitor ongoing behavioral and physical health conditions and HRSNs. In this value-based care approach, the practice participants will be compensated based on the quality of care provided and improved patient outcomes.
Highlights |
|---|
|
Model Purpose
Medicaid populations experience disproportionately high rates of mental health conditions and/or substance use disorders (SUD) and account for nearly half of all Medicaid expenditures. Medicare populations also experience higher than average rates of mental illness and/or SUD. Consequently, both populations are more likely to experience frequent visits to the emergency department and hospitalizations, have poor health outcomes, and premature death.
Limited access to care, stigma, and untreated or poorly managed chronic conditions like diabetes and heart disease can contribute to worsening health outcomes for these populations. Behavioral health providers face significant barriers to delivering care due to a lack of resources and a fragmented health care delivery system that does not systematically integrate behavioral and physical health care. The IBH Model aims to help participating practices improve access to and promote high-quality integrated care. By supporting behavioral health practices to lead an interprofessional care team, the model will address patients’ behavioral and physical health and health-related social needs.
Model Design
IBH is a state-based model focused on community-based behavioral health practices that treat Medicaid and Medicare beneficiaries and includes both Medicaid and Medicare-aligned payment models. CMS will first issue awards to Medicaid agencies in up to eight states to implement the model. Practice participants within selected states may volunteer to participate in the Medicare payment model. The selected states will partner with their state’s agencies for mental health and/or SUD to ensure alignment in clinical policies, as well as work with at least one partnering Medicaid Managed Care Organization (MCO) or another intermediary partner, where applicable, to develop and implement the IBH Model in their state.
IBH supports behavioral health practices in delivering integrated care in outpatient settings. This person-centered approach to addressing whole-person health represents a “no wrong door” approach that prioritizes close collaboration with primary care and other physical health providers to support all aspects of a patient’s care.
Community-based behavioral health practices (“practice participants”) will be responsible for conducting screenings and assessments of behavioral and physical health and health-related social needs, offering treatment as appropriate within their scope of practice, providing “closed loop” referrals to other primary care providers, specialists, and community-based resources, and monitoring ongoing conditions. Since people with moderate to severe behavioral health conditions frequently visit behavioral health settings, this approach uses the behavioral health setting as a point of entry to identify and secure further care and facilitate close collaboration with primary and specialty care providers.
The model works to improve care through four key program pillars:
- Care Integration: Behavioral health practice participants will screen, assess, refer, and treat patients, as needed, for the services they require.
- Care Management: An interprofessional care team, led by the behavioral health practice participant, will identify, and as appropriate address, the multi-faceted needs of patients and provide ongoing care management.
- Health Equity: Behavioral health practice participants will conduct screenings for HRSNs and refer patients to appropriate community-based services. Participating practices will be required to develop a health equity plan (HEP). The HEP should stipulate how the practice participant will address disparities that impact their service populations.
- Health Information Technology: Expansion of health IT capacity through targeted investments in interoperability and tools (including electronic health records) will allow participants to improve quality reporting and data sharing.
The IBH Model is projected to run for eight years and includes a pre-implementation period (model years 1-3). During this period, states and practice participants will receive funding to develop and implement model activities and capacity building. During model year 1, states will conduct outreach and recruit behavioral health practice participants into the model. Practice participants will receive funding to support necessary upgrades to health IT and electronic health records, as well as practice transformation activities, and staffing to implement the model. Practice participants who elect to participate in the Medicare payment model may also be eligible for additional funding to support model activities.
By the start of model year 4, states will implement a Medicaid payment model that supports practice participants in implementing the care delivery framework. Practice participants in selected states who participate in the additional Medicare payment model will receive a per-beneficiary-per-month payment to support their implementation of the care delivery framework. These payments will be further supplemented with additional performance-based payments during the implementation period (model years 4-8). Additional information about eligibility to receive these payments will be provided in the NOFO.
This model is intended to prepare practices for more advanced alternative payment models and accountable care arrangements in the future.
Eligibility Criteria
CMS will award Cooperative Agreements to up to eight state Medicaid agencies (SMAs), through a Notice of Funding Opportunity (NOFO) to participate in the IBH Model.
States, including U.S. territories and the District of Columbia, have the option to apply as a whole state, or a specified sub-state region. If selected, a participating state is required to select practice participants – community-based behavioral health organizations or settings that, at the time of application, meet all the following criteria:
- Are licensed by the state awardee to deliver behavioral services, either mental health and/or substance use disorders
- Meet all state-specific Medicaid provider enrollment requirements
- Are eligible for Medicaid reimbursement
- Serve adult Medicaid beneficiaries (age 18 or older) with moderate to severe behavioral health conditions
- Provide mental health and/or substance use disorder services at the outpatient level of care
Medicare and Medicaid beneficiaries, including those dually eligible, who receive behavioral health care from a participating practice are eligible to receive services as part of the model. All applications will be reviewed by a panel of technical experts.
Health Equity Strategy
The IBH Model supports CMS’ broader efforts to promote health equity and ensure all populations can achieve optimal health outcomes.
People with mental health conditions and/or substance use disorder often experience health disparities. These health disparities are further exacerbated among historically marginalized racial and ethnic groups, low-income, and/or rural populations.
Practice participants are required to create a Health Equity Plan (HEP) using a needs assessment of the population they serve. The HEP should detail steps that practice participants will take to address the population needs and stipulate how the practice participant will address disparities that disproportionately impact their service populations.
Additionally, the IBH Model will require practice participants to annually screen and monitor patients for underlying and/or unmet HRSNs and make necessary referrals to other health care providers or local safety-net services, and that the required care management component will help ensure that Medicaid beneficiaries receive the services needed to address their health-related social needs.
Events
Additional Information
- IBH Model Fact Sheet (PDF)
- IBH Model Press Release
- IBH Model Fact Sheet on Model Benefits for State Medicaid Agencies (PDF)
- IBH Model Patient Journey Map (PDF)
- IBH Model Frequently Asked Questions
Outreach
If you are interested in receiving additional information, updates, or have questions about the Innovation in Behavioral Health Model, please see the resources below:
- Email: IBHModel@cms.hhs.gov
- Sign Up for email updates from the Innovation in Behavioral Health Model team