What’s Changed?
We updated the enrollment application fee amount for 2026.
Substantive content changes are in dark red.
Application Fee
Physicians, non-physician practitioners (NPPs), physician organizations, non-physician organizations, and Medicare Diabetes Prevention Program (MDPP) suppliers don’t pay a Medicare enrollment application fee.
Generally, institutional providers and suppliers like DMEPOS suppliers and opioid treatment programs pay an application fee when enrolling, re-enrolling, revalidating, or adding a new practice location.
Enrollment Application Fee
The 2026 enrollment application fee is $750.
Enrollment
Providers must enroll in the Medicare Program to get paid for providing covered services to Medicare patients. Determine if you’re eligible to enroll and how to complete enrollment.
Step 1: Get an NPI
To enroll in the Medicare Program, get an NPI through:
- Online Application: Get an Identity & Access Management (I&A) System user account. Then apply for an NPI in NPPES.
- Paper Application: Complete, sign, and mail the National Provider Identifier (NPI) Application/Update Form (CMS-10114) paper application to the NPI Enumerator address on the form. To request a hard copy application:
- Call 1-866-484-8049 (TTY 1-866-523-4759)
- Email EUS_Support@cms.hhs.gov
- Bulk Enumeration: Apply for Electronic File Interchange access and upload your own CSV or XML files.
Not Sure If You Have an NPI?
Search for your NPI on the NPPES NPI Registry.
CMS Provider Enrollment Systems:
Multi-Factor Authentication
To better protect your information, we implemented I&A System multi-factor authentication for the provider enrollment systems.
Step 2: Complete Proper Medicare Enrollment Application
After you get an NPI, you can:
- Complete Medicare Program enrollment
- Revalidate your enrollment
- Change your enrollment information
Before applying, get the necessary enrollment information and complete the actions using PECOS or the paper enrollment form.
A. Online PECOS Application
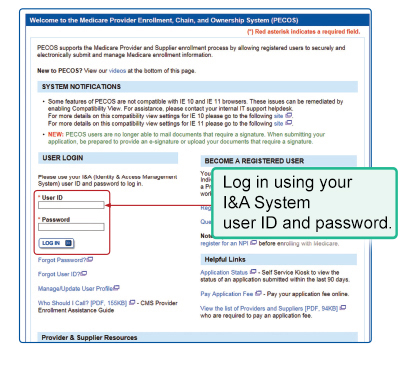
After we approve your I&A System registration, submit your PECOS application.
PECOS offers a scenario-driven application, asking questions to recover the information for your specific enrollment scenario. You can use PECOS to submit all supporting documentation. Follow these instructions:
- Log in to PECOS.
- Continue with an existing enrollment or create a new application.
- When PECOS determines your enrollment scenario, and you confirm it’s correct, you’ll see the topics for submitting your application. To complete each topic, enter the necessary information.
- At the end of the data entry process, PECOS:
- Confirms you entered all necessary data
- Lists MAC documents to submit for review
- Gives the option to electronically sign and certify
- Shows your MAC’s name and mailing address
- Lets you print your enrollment application for your records (don’t submit a paper copy to your MAC)
- Sends the application electronically to your MAC
- Emails you to confirm your MAC got the application
PECOS Scroll Functionality
PECOS validates that you’ve read and acknowledged certification terms and conditions before you electronically submit your Medicare enrollment application. Review and scroll through each text box with certification requirements before you select accept on these pages:
- Submission
- Home
- Remote E-sign
B. Paper Medicare Enrollment Applications
Submit the appropriate paper enrollment application if you’re unable to use PECOS. Carefully review the paper application instructions to decide which form is right for your practice. The paper enrollment application collects your information, including documentation verifying your Medicare Program enrollment eligibility.
If you submit a paper application, your MAC processes your application and creates a Medicare enrollment record by entering the data into PECOS.
Step 3: Respond to Requests for More Information
MACs pre-screen and verify enrollment applications for completeness. Respond to MAC information requests within 30 days. If you don’t, the MAC may reject your application.
Your MAC won’t fully process your PECOS enrollment application without your electronic or uploaded signature, application fee (if applicable), and necessary supporting documentation. The enrollment application filing date is when the MAC gets your enrollment application.
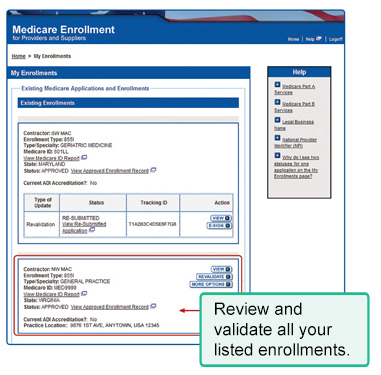
You can check your PECOS enrollment application status 2 ways:
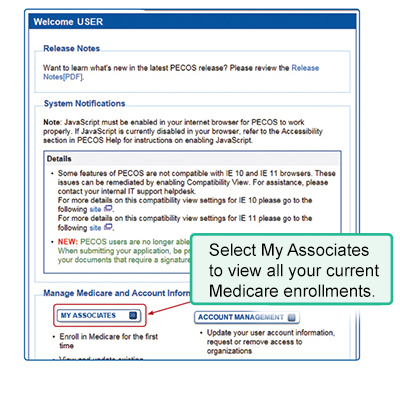
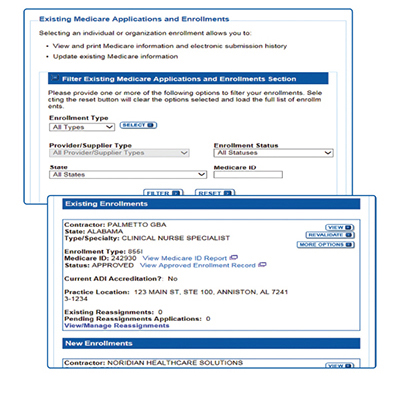
- Log in to PECOS and select the View Enrollments link. In the Existing Enrollments section, find the application. The system shows the application status.
- To see your enrollment status without logging in, go to PECOS and, under Helpful Links, select Application Status.
When your MAC approves your application, it switches the PECOS record to an approved status and sends you an approval letter.
Provider Enrollment Site Visits
We conduct a site visit verification process using National Site Visit Contractors (NSVCs). A site visit helps prevent questionable providers and suppliers from enrolling or staying enrolled in the Medicare Program.
The NSVCs conduct unannounced site visits for all Medicare Parts A and B providers and suppliers, including DMEPOS suppliers. The NSVCs may conduct an observational site visit or a detailed review to verify enrollment-related information and collect other details based on pre-defined CMS checklists and procedures.
During an observational visit, the inspector has minimal contact with the provider or supplier and doesn’t hinder the facility’s daily activities. The inspector will take facility photos as part of the site visit. During a detailed review, the inspector enters the facility, speaks with staff, and collects information to confirm the provider’s or supplier’s compliance with our standards.
Inspectors performing site visits have a photo ID and a CMS-issued, signed authorization letter the provider or supplier may review. If you or your staff want to verify that we ordered a site visit, contact your MAC.
Make your office staff aware of the site visit verification process. An inspector’s inability to perform a site visit may result in denial of your Medicare enrollment application or revocation of your Medicare billing privileges.
Step 4: Use PECOS to Keep Enrollment Information Current
Report a Medicare enrollment change using PECOS. Physicians, NPPs, and physician and NPP organizations must report a change of ownership or control (including a change in authorized official, delegated official, or managing employee), a change in practice location, and any final adverse legal actions (like a felony or suspension of a federal or state license) within 30 days and report all other changes within 90 days.
DMEPOS suppliers must report changes in their enrollment application information within 30 days.
Independent diagnostic testing facilities must report changes in ownership, location, general supervision, and adverse legal actions within 30 days and report all other changes within 90 days.
MDPP suppliers must report changes in ownership (including the authorized official, delegated official, or managing employee), changes to the coach roster, and final adverse legal actions within 30 days and report all other changes, including changes in location, within 90 days.
PECOS Users
We allow various organizations and users to work in our systems. The type of user depends on their relationship with you and the duties they perform in your practice.
You may choose other users to act for your organization to manage connections and staff, including appointing and approving other system-authorized users. Depending on your professional relationships with other providers, the CMS External User Services Help Desk may ask you for more validation information.
One Account, Multiple Systems
We use several provider enrollment systems. Organizational providers and suppliers must use the Identity & Access Management (I&A) System to name an Authorized Official (AO) to work in CMS systems. The I&A System allows you to:
- Use NPPES to apply for and manage NPIs
- Use PECOS to enroll in Medicare or update or revalidate your current enrollment information
- Register to get Medicare Promoting Interoperability Program payments for eligible professionals and hospitals that adopt, use and upgrade, or show meaningful use of electronic health record (EHR) technology
Authorized Officials, Access Managers, Staff End Users & Surrogates
Organizational providers or suppliers must appoint and authenticate an AO through the I&A System to work in PECOS for them. That person must meet the AO regulatory definition. For example, an AO is a chief executive officer, chief financial officer, general partner, chair of the board, or direct owner who can legally enroll in the Medicare Program.
Respond to your employer’s AO invitation or initiate the request yourself. After you’re the confirmed AO, use PECOS for your provider or supplier organization. As an AO, you’re responsible for approving PECOS user system requests to work on behalf of the provider or supplier organization. Regularly check your email and take the requested actions.
AOs may delegate their responsibilities to an Access Manager who can also initiate or accept connections and manage staff for their organizations.
AOs or Access Managers may invite a Staff End User (SEU) or Surrogate to access PECOS for their organization. Once registered, an SEU or Surrogate may log in to access, view, and modify CMS system information, but they can’t represent the practice, manage staff, sign enrollment applications, or initiate or accept connections.
| Role | Represent an Organization | Manage Staff | Approve or Manage Connections | Act on Behalf of Provider in CMS Systems |
|---|---|---|---|---|
| Individual Provider | Yes | Yes | Yes | Yes |
| AO | Yes | Yes | Yes | Yes |
| Access Manager | Yes | Yes | Yes | Yes |
| SEU | No | No | No | Yes |
| Surrogate | No | No | No | Yes |
We recommend using the same I&A System-appointed AO and PECOS Access Managers. The assigned AO and Access Managers must have the right to legally bind the company and be responsible for approving the system staff and be CMS-approved in the I&A System.
Only AOs can sign an initial organization enrollment application. An Access Manager can sign changes, updates, and revalidations.
The I&A System Quick Reference Guide instructs you on managing system users.
PECOS Technical Help
Using PECOS may require technical support. The first step toward a solution is knowing which CMS contractor to contact.
Common Problems & Who to Contact
PECOS FAQs
Application Fee & Supporting Documentation
Enrollment Application Issues
Submitting Reportable Events
Revalidations
Revalidation means resubmitting and recertifying your enrollment information.
Protect Your Identity & Privacy
You can help protect your professional medical identifiers from identity thieves attempting to defraud the Medicare Program.
Keep PECOS Enrollment Information Current
Log in to PECOS and review your Medicare enrollment information several times a year to make sure there are no unauthorized changes.
PECOS Provides Security
Only you, authorized surrogates, authorized CMS officials, and Medicare Administrative Contractors (MACs) may enter and view your Medicare PECOS enrollment information. CMS officials and MACs get security standards training and must protect your information. We don’t disclose your Medicare enrollment information to anyone, except when authorized or required by law.
Review & Protect Enrollment Information
Review your Medicare enrollment information in PECOS frequently to make sure it’s accurate, current, and unaltered.
Use your Identity & Access Management (I&A) System user ID and password to access PECOS. Keep your ID and password secure.
Protect Yourself & CMS Programs from Fraud
Your NPI and employer identification number (EIN) are publicly available information. Use extra caution to monitor and protect your professional and personal information to help prevent fraud and abuse. Also make sure your patients’ personal health information is secure. Refer to these resources:
Take these steps to verify your Medicare enrollment information:
Step 5: Report Identity Theft, If Needed
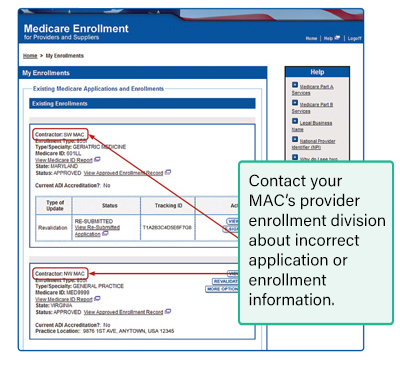
If you suspect your PECOS profile is incorrect due to unauthorized account access, contact your MAC, law enforcement authorities, and your bank. Your MAC and bank can flag your respective accounts for possible fraudulent activity, and law enforcement can start investigating if and how your accounts were compromised.
Additional Privacy Tips
Take these additional actions to protect your Medicare enrollment information:
- Change your password in the I&A System before accessing PECOS the first time. You can’t change your user ID, but you must change your password every 60 days.
- Review your Medicare enrollment information several times a year to make sure no one changed information without your knowledge. Immediately report changes you didn’t submit.
- Maintain your Medicare enrollment record. Report Medicare enrollment changes known as reportable events, including change of ownership or control, change in practice location, change in banking arrangements, and any final adverse legal actions.
- Store PECOS copies or paper enrollment applications in a secure location. Don’t allow others access to this information, as it contains your personal information, including your date of birth and SSN. Don’t leave copies in a public workspace.
- Enroll in electronic Medicare payments and make sure they deposit directly into your bank account. We require all providers to use electronic funds transfer (EFT) when enrolling in Medicare, revalidating, or making changes to their enrollment. The most efficient way to enroll in EFT is to complete the EFT information section in PECOS and provide the required supporting documentation. Using EFT allows us to send payments directly to your bank account.
DMEPOS Supplier Requirements
DMEPOS Supplier Standards, Accreditation & Surety Bond
To enroll in Medicare or keep your Medicare billing privileges, all DMEPOS suppliers (except certain exempted professionals) must meet supplier and DMEPOS quality standards to become accredited. Certain DMEPOS suppliers must also submit a surety bond.
DMEPOS suppliers (except those exempted eligible professionals and other persons) must be accredited by a CMS-approved accrediting organization before submitting a Medicare enrollment application to the National Provider Enrollment (NPE) DMEPOS contractors.
Each enrolled DMEPOS supplier covered under the Health Insurance Portability and Accountability Act (HIPAA) must name each practice location (if it has more than 1) as a subpart and make sure each subpart gets its own NPI.
Individual DMEPOS Suppliers (for example, sole proprietorships)
Physicians, non-physician practitioners (NPPs), and DMEPOS suppliers may use their Identity & Access Management (I&A) System user ID and password to access PECOS. If you don’t already have an I&A System account, refer to the I&A System User Registration page and enter the information to open an account. For help, refer to the How to Setup Your Account if you are a Sole Owner section in the I&A System Quick Reference Guide.
As an individual DMEPOS supplier, you don’t need an Authorized Official (AO) or another authorized user.
Organizational DMEPOS Suppliers System Users
A DMEPOS supplier organization must appoint an AO to manage connections and staff, including appointing and approving other authorized PECOS users. The organization must identify the AO in the enrollment application. The AO must have ownership or managing control in the DMEPOS supplier organization.
Providers Who Solely Order or Certify
Physicians and other eligible professionals must enroll in the Medicare Program or have a valid opt-out affidavit on file to solely order or certify Medicare patient items or services.
Those physicians and other eligible professionals enrolled solely as ordering/certifying providers don’t send billed service claims to a Medicare Administrative Contractor (MAC).
Ordering/Certifying Terms
Medicare Part B claims use the term ordering/certifying provider to identify the professional who orders or certifies an item or service reported in a claim. These are technically correct terms:
- Providers order non-physician patient items or services, like DMEPOS, clinical lab services, or imaging services
- Providers certify patient home health services
The health care industry uses the terms ordered, referred, and certified interchangeably.
Who Are Eligible Ordering/Certifying Providers?
Physicians or eligible professionals who order or certify Medicare Part A or B services but don’t want to submit Medicare claims are eligible ordering/certifying providers.
A person already enrolled as a Part B provider may submit claims listing themselves as the ordering/certifying provider without re-enrolling using Medicare Enrollment Application: Enrollment for Eligible Ordering/Certifying Physicians and Other Eligible Professionals (CMS-855O).
Note: Those who enroll as eligible providers using CMS-855O can’t bill Medicare, and we can’t pay for their services because they have no Medicare billing privileges.
Organizational NPIs don’t qualify, and you can’t use them to order or certify.
Eligible providers must meet these basic conditions:
- Have an individual NPI
- Be enrolled in Medicare in either an approved or opt-out status
- Be an eligible specialty type to order or certify
Denial of Ordering/Certifying Claims
If claims lack a valid individual NPI, MACs deny them if they’re from:
- Clinical labs for ordered tests
- Imaging centers for ordered imaging procedures
- DMEPOS suppliers for ordered DMEPOS
- Part A home health agencies that aren’t ordered or certified by a Doctor of Medicine, Osteopathy, or Podiatric Medicine
- Part A hospices that aren’t certified by a Doctor of Medicine or Osteopathy
If you bill a service that needs an eligible provider and they aren’t on the claim, the MAC will deny the claim. The claim must have a valid NPI and the eligible provider’s name as it appears in PECOS.
If a provider who’s on the Preclusion List prescribes a Medicare Part D drug, drug plans will deny it.
Requirement 1: Get an Individual NPI
The 2 types of NPIs are: Type 1 (individual) and Type 2 (organizational). Medicare allows only Type 1 NPIs to solely order items or certify services. Apply for an NPI through:
- Online Application: Get an Identity & Access Management (I&A) System user account. Then apply for an NPI in NPPES.
- Paper Application: Complete, sign, and mail the National Provider Identifier (NPI) Application/Update Form (CMS-10114) paper application to the NPI Enumerator address on the form. To request a hard copy application:
- Call 1-866-484-8049 (TTY 1-866-523-4759)
- Email EUS_Support@cms.hhs.gov
- Bulk Enumeration: Apply for Electronic File Interchange access and upload your own CSV or XML files.
Requirement 2: Enroll in Medicare in an Approved or Opt-Out Status
Once you have an NPI, use PECOS to verify current Medicare enrollment record information, including your NPI and that you’re approved, or go to the Opt Out Affidavits list to check your status. To opt out of Medicare, submit an affidavit expressing your decision to opt out of the Program.
Part C and Part D providers don’t have to enroll in Medicare in an approved or opt-out status.
| Verification Option | Enrollment Record Is Current If: |
|---|---|
| Go to the Order and Referring datasets* | You’re on 1 of these reports |
| Go to PECOS to find your enrollment record | Your enrollment record displays an approved status |
| If you submitted an enrollment application as 1 of the eligible provider types on paper (CMS-855O) or using PECOS and want to check the status, go to the Pending Initial Logging and Tracking Non Physicians and Pending Initial Logging and Tracking Physicians datasets | Your enrollment application is pending contractor review and you’re on 1 of these reports |
* We deny certain power mobility device claims if the ordering provider isn’t on our eligible providers list.
Requirement 3: Be Eligible to Order or Certify
The physicians and eligible professionals who may enroll in Medicare solely for ordering or certifying include, but aren’t limited to, physicians and eligible professionals who are:
- Department of Veterans Affairs employees
- Public Health Service employees
- Department of Defense or TRICARE employees
- Indian Health Service or Tribal Organization employees
- Federally Qualified Health Center, Rural Health Clinic, or Critical Access Hospital employees
- Licensed residents in an approved medical residency program as defined in 42 CFR 413.75(b)
- Dentists, including oral surgeons
- Pediatricians
- Retired, licensed physicians
If you’re unsure whether your specific provider specialty qualifies to enroll as an ordering/certifying provider, refer to Section 4 of CMS-855O or find your MAC’s website before submitting a Medicare enrollment application.
See provider specialty codes for dentists.
Interns & Residents
Claims for items or services ordered or certified by licensed or unlicensed interns and residents must specify a teaching physician’s NPI and name. State-licensed residents may enroll to order or certify and can be listed on claims. If states offer provisional licenses or otherwise permit residents to order or certify, we allow interns and residents to enroll consistent with state law.
Requirement 4: Respond to Requests for More Information
MACs pre-screen and verify enrollment applications for completeness. If the MAC needs more information, respond to information requests within 30 days. If you don’t, the MAC may reject your application.
Your MAC won’t fully process your PECOS enrollment application without your electronic or uploaded signature, application fee (if applicable), and necessary supporting documentation. The enrollment application filing date is when the MAC gets your enrollment application.
You can check your PECOS enrollment application status 2 ways:
- Log in to PECOS and select the View Enrollments link. In the Existing Enrollments section, find the application. The system shows the application status.
- To see your enrollment status without logging in, go to PECOS and, under Helpful Links, select Application Status.
When your MAC approves your application, it switches the PECOS record to an approved status and sends you an approval letter.
Requirement 5: Use PECOS to Keep Enrollment Information Current
Report a Medicare enrollment change using PECOS. Providers and suppliers must report a change of ownership or control (including a change in authorized official, delegated official, or managing employee), a change in practice location, and any final adverse legal actions (like revocation or suspension of a federal or state license) within 30 days and must report all other changes within 90 days.
DMEPOS suppliers must report changes in their enrollment application information within 30 days.
Independent diagnostic testing facilities must report changes in ownership, location, general supervision, and adverse legal actions within 30 days and report all other changes within 90 days.
Medicare Diabetes Prevention Program suppliers must report changes in ownership (including the authorized official, delegated official, or managing employee), changes to the coach roster, and final adverse legal actions within 30 days and report all other changes, including changes in location, within 90 days.
Revalidation
Revalidation, or resubmitting and recertifying your enrollment information’s accuracy, is an important anti-fraud tool. All Medicare-enrolled providers and suppliers must periodically revalidate their enrollment information.
Generally, physicians, including physician organizations, opioid treatment programs, Medicare Diabetes Prevention Program suppliers, and institutional providers, revalidate enrollment every 5 years or when we request it. DMEPOS suppliers must revalidate their enrollment information every 3 years or when we request it.
PECOS is the most efficient way to revalidate information.
If you’re actively enrolled, go to the Medicare Revalidation List to find your revalidation due date. If you see a due date, submit your revalidation before that date. Your Medicare Administrative Contractor (MAC) notifies you when it’s time to revalidate. If you submit your revalidation application after the due date, your MAC may hold your Medicare payments or deactivate your billing privileges.
Rebuttal Process
MACs issue Medicare billing privilege deactivations. We permit providers and suppliers to file a rebuttal.
Get more information:
Large Group Coordination
Groups with more than 200 members can use the Medicare Revalidation List and search by their organization’s name to download group information. Their MAC will send them a letter and spreadsheet that lists the providers linked to their group who must revalidate within 6 months. Large groups should work together to make sure they submit only 1 application from each provider or supplier.
Resources
Use these resources to learn how to enroll in the Medicare Program, revalidate your enrollment, or change your enrollment information. Enroll in the Medicare Program to get paid for providing covered patient services. Enroll if you solely order items or certify services.
You can enroll online by using PECOS or the appropriate paper enrollment application you submit to your MAC.
- Get an Identity & Access Management (I&A) System user account
- Apply for your NPI in NPPES
- Enroll in PECOS
| Topic | Title |
|---|---|
| Application fee | Application Fee Requirements for Institutional Providers |
| Provider-supplier general information | Become a Medicare Provider or Supplier |
| Topic | Title |
|---|---|
| Revalidation due dates | Medicare Revalidation List |
| Revalidation overview | Revalidations (Renewing Your Enrollment) |
| Topic | Title |
|---|---|
| FAQs | PECOS FAQs |
| Get an NPI | What’s New in NPPES 3.0 (video) |
| Online enrollment system | PECOS |
| PECOS tutorials | PECOS Enrollment Tutorial Videos |
| Register for user IDs and passwords to access NPPES, PECOS, and the EHR incentive program |
I&A System Quick Reference Guide I&A FAQs |
| Search NPI records, including the provider’s name, specialty, and practice address | NPPES NPI Registry |
| Submit provider NPI applications and update information electronically in NPPES | Electronic File Management Main Page |
| Topic | Contact |
|---|---|
| Application for NPI | NPPES Home Page/Sign In Page Help |
| Institutional and other providers state survey | Contact Information for State Survey Agencies |
| Navigating and accessing PECOS website | CMS External User Services (EUS) Help Desk “Who should I call?” CMS Provider Enrollment Assistance Guide |
| Paper applications | Medicare Fee-for-Service Provider Enrollment Contact List |
| Provider site visit | Become an Institutional Provider |
| All other enrollment-related questions | Find your MAC’s website |
Enrollment Forms
If you enroll using a paper application instead of PECOS, search the CMS Forms List to find the form you need and read on page 1, Who Should Submit This Application.
| Form | Form Number |
|---|---|
| Electronic Funds Transfer (EFT) Authorization Agreement | CMS-588 |
| Medicare Enrollment Application: Clinics/Group Practices and Other Suppliers | CMS-855B |
| Medicare Enrollment Application: Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Suppliers | CMS-855S |
| Medicare Enrollment Application: Enrollment for Eligible Ordering/Certifying Physicians and Other Eligible Professionals | CMS-855O |
| Medicare Enrollment Application: Institutional Providers | CMS-855A |
| Medicare Enrollment Application: Medicare Diabetes Prevention Program (MDPP) Suppliers | CMS-20134 |
| Medicare Enrollment Application: Physicians and Non-Physician Practitioners | CMS-855I |
| Medicare Participating Physician or Supplier Agreement | CMS-460 |
| National Provider Identifier (NPI) Application/Update Form | CMS-10114 |
| Health Insurance Benefit Agreement | CMS-1561 |
Commonly Used Terms
- CMS
- CMS is the federal agency that administers the Medicare, Medicaid, Children’s Health Insurance Program (CHIP), Health Insurance Portability and Accountability Act (HIPAA), Clinical Laboratory Improvement Amendments (CLIA), and several other health-related programs.
- CMS-460
- The Medicare Participating Physician or Supplier Agreement describes your willingness to accept assignment for all covered services you provide to patients. If you participate, we pay 5% more, and participating providers get timely, direct payment.
- CMS-588
- The Electronic Funds Transfer (EFT) Authorization Agreement tells you how to get electronic payments or update existing banking information.
- CMS-855A
- The Medicare enrollment application that institutional providers use to enroll, revalidate enrollment, or change enrollment information.
- CMS-855B
- The Medicare enrollment application that clinics or group practices and other suppliers (except DMEPOS suppliers) use to enroll, revalidate enrollment, or change enrollment information.
- CMS-855I
- The Medicare enrollment application that physicians and non-physician practitioners (NPPs) (individual physicians or NPPs) use to enroll, revalidate enrollment, or change enrollment information. Physicians and NPPs can also reassign their right to bill the Medicare Program, terminate a current reassignment of Medicare benefits, or make a change in their reassignment of Medicare benefit information using the CMS-855I.
- CMS-855O
- The Medicare enrollment application that eligible ordering, certifying, and prescribing physicians and other eligible professionals (physicians, including dentists and other eligible NPPs) use to enroll solely to order items or certify patient services. This includes those physicians and other eligible NPPs who don’t and won’t send patient service claims to a MAC.
- CMS-855S
- The Medicare enrollment application that DMEPOS suppliers use to enroll, revalidate enrollment, or change enrollment information.
- CMS-1561
- The Health Insurance Benefit Agreement is an agreement between a provider and CMS to get Medicare payments.
- CMS-10114
- This form tells you how to apply for an NPI or submit updates.
- CMS-20134
- The Medicare enrollment application that Medicare Diabetes Prevention Program suppliers use to enroll, revalidate enrollment, or change enrollment information.
- Director
- A director of a corporation, even when the provider or supplier is a non-profit entity. This includes any member of the corporation’s governing body regardless of the board’s or member’s specific title. The body could be a board of directors, board of trustees, or something similar.
- DMEPOS Suppliers
- Entities or persons, including physicians or Part A providers, who sell or rent Part B covered items to patients and meet the DMEPOS supplier standards.
- Electronic File Interchange (EFI)
- The EFI process lets CMS-approved EFI Organizations electronically submit provider NPI applications and update NPPES information with minimal manual intervention.
- Electronic Funds Transfer (EFT)
- We directly pay EFT providers by sending payments to the provider’s financial institution whether they file claims electronically or on paper. All our providers must apply for EFT.
- Electronic Health Record (EHR)
- An EHR is an electronic version of a patient’s medical history.
- External User Services (EUS) Help Desk
- EUS is a dedicated CMS online support site offering help, including, but not limited to, the I&A System, PECOS, and NPPES.
- Identity & Access Management (I&A) System
- Users register for user IDs and passwords to access PECOS, NPPES, and the Medicare Promoting Interoperability Program.
- Institutional Provider
- These are providers or suppliers that submit a CMS-855A, CMS-855B (except physician and NPP organizations), or CMS-855S form. See page 1 of the respective provider-type forms to learn who should use them.
- Managing Organization
- An entity that exercises operational or managerial control over, or directly or indirectly conducts, the day-to-day operations of the provider or supplier, either under contract or through some other arrangement.
- Medicare Administrative Contractor (MAC)
- A private company that contracts with us to process and pay Fee-for-Service patient Parts A and B medical or DME claims.
- Medicare Application Fee
- Institutional providers and suppliers must pay an application fee when they initially enroll in Medicare, add a practice location, or revalidate their enrollment information. We define an institutional provider as any provider or supplier that submits a CMS-855A, CMS-855B (except physician and NPP organizations), or CMS-855S form.
- NPPES
- NPPES assigns unique NPIs to Medicare providers and health plans to improve the efficiency and effectiveness of electronically submitting health information.
- National Site Visit Contractor (NSVC)
- The NSVC performs a site visit to screen and stop questionable providers and suppliers from enrolling or maintaining enrollment.
- NPI Enumerator
- The NPI Enumerator helps Medicare providers apply for NPIs and update their information in NPPES.
- NPI Registry
- The NPI Registry is a directory of all active NPI records that displays relevant public portions of the record, including the provider’s name, specialty, and practice address.
- Officer
- An officer of a corporation, regardless of whether the provider or supplier is a non-profit entity.
- Participating Physician or Supplier
- Participating physicians or suppliers agree to accept patient assignment on Medicare service claims. They agree to accept allowed amounts as payment in full and to collect only the deductible and coinsurance or copayment. See CMS-460.
- PECOS
- PECOS is CMS’s online provider enrollment system allowing registered users to securely and electronically submit and manage enrollment information. You can use PECOS instead of paper enrollment forms.
- Reassignment of Medicare Benefits
- Reassigning your Medicare benefits lets an eligible organization or group submit claims and get payment for Part B services you provide as a member of an organization or group. See CMS-855I.
- Revalidation
- A provider and supplier mandatory resubmission and recertification process to maintain enrollment information accuracy and Medicare billing privileges. The process ensures enrollment information on file remains complete and current and helps fight health care fraud.
- State Survey Agencies
- They perform initial surveys and periodic resurveys of all institutional providers (including labs) and certain kinds of suppliers. These surveys determine if a provider or supplier meets the conditions to participate in the Medicare Program and evaluate their performance and quality of care.
View the Medicare Learning Network® Content Disclaimer and Department of Health & Human Services Disclosure.
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department of Health & Human Services (HHS).