CMS achieved improper payment rate reductions in Medicare Fee-For-Service (FFS),
Medicare Part C, Medicare Part D, Medicaid, and Children’s Health Insurance Program
Medicare FFS improper payment rate is at its lowest since 2010
CMS remains steadfast in its commitment to reduce improper payments by focusing on identifying, reporting, and implementing actions to reduce payment error vulnerabilities. CMS has implemented several initiatives to address improper payments, resulting in this being the first year in improper payment reporting history that the Medicare Fee-For-Service (FFS), Medicare Part C, Medicare Part D, Medicaid and Children’s Health Insurance Program achieved reductions in all five programs’ improper payment rates.
Most notably, the 2018 Medicare FFS improper payment rate is 8.12 percent. This is the lowest Medicare FFS improper payment rate since 2010 and the second consecutive year that the Medicare FFS improper payment rate is below the 10 percent threshold for compliance established in the Improper Payments Elimination and Recovery Act of 2010.
Due to the successes of CMS’ actions to address improper payments in home health and skilled nursing facility claims, CMS has achieved a decrease in the Medicare FFS improper payment rate from 9.51 percent in 2017 to 8.12 percent in FY 2018. This represents a $4.59 billion decrease in estimated improper payments from 2017 to 2018. The 2018 Medicare FFS estimated improper payment rate represents claims processed between July 1, 2016 and June 30, 2017.
CMS employs multi-faceted efforts to target the root causes of improper payments, with an emphasis on prevention-oriented activities. Actions to prevent and reduce improper payments include: policy clarifications and simplifications; prior authorization initiatives that ensure applicable coverage, payment, and coding rules are met before services are rendered; a targeted probe and educate medical review strategy that focuses on outlier providers, limits the number of medical records requested, and puts emphasis on education and assistance in correcting claims errors; and provider education on Medicare policy.
Home health corrective actions resulted in a significant $6.92 billion decrease in estimated improper payments from 2015 to 2018. The home health improper payment rate decreased from 58.95 percent in 2015 to 17.61 percent in 2018.
Fiscal Year (FY) 2015-2018 Medicare FFS Overall and Home Health Improper Payment Rates

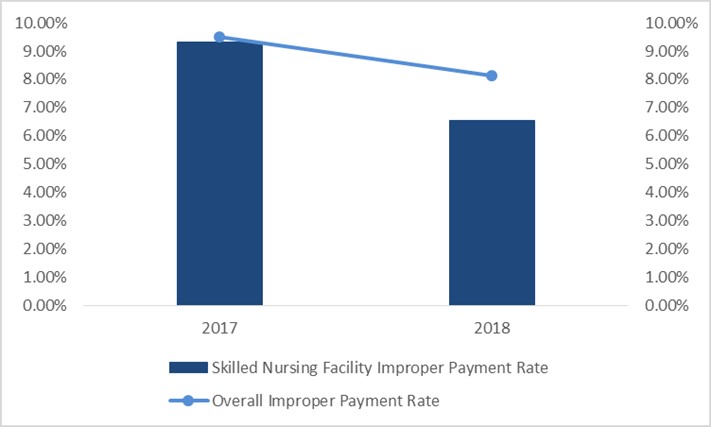
Skilled nursing facility corrective actions resulted in a $1.04 billion decrease in estimated improper payments from 2017 to 2018. The skilled nursing facility improper payment rate decreased from 9.33 percent in 2017 to 6.55 percent in 2018.
FY 2017-2018 Medicare FFS Overall and Skilled Nursing Facility Improper Payment Rates
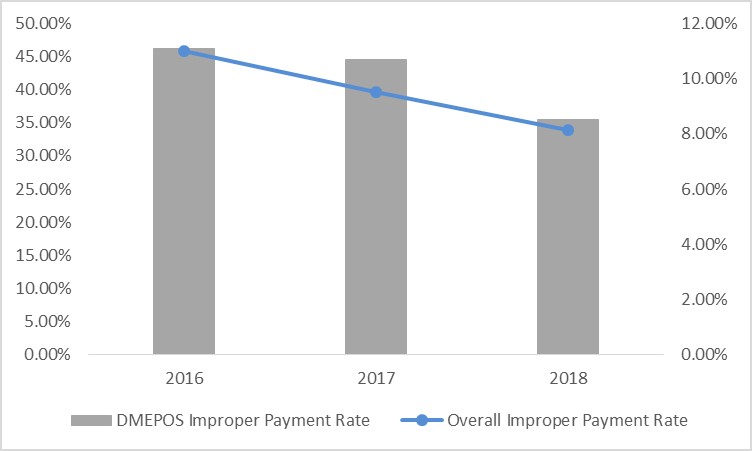
The Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) improper payment rate decreased from 46.26 percent in 2016 to 35.54 percent in 2018. While DMEPOS represents a small portion of total improper payments, DMEPOS corrective actions resulted in a $1.14 billion decrease in estimated improper payments from 2016 to 2018.
FY 2016-2018 Medicare FFS Overall and DMEPOS Improper Payment Rates
CMS is pleased to have achieved this decline in the Medicare FFS improper payment rate and continues to explore additional opportunities to reduce the improper payment rate. We remain committed to collaborating across CMS and with stakeholders to address potential vulnerabilities, strengthen our program integrity efforts, and minimize unnecessary administrative burden for our partners.
###
Get CMS news at cms.gov/newsroom, sign up for CMS news via email and follow CMS on Twitter CMS Administrator @SeemaCMS, @CMSgov, and @CMSgovPress.