We make updates to IPPS payment rates, including updates to base rates, wage indexes, Medicare Severity Diagnosis Related Group (MS-DRG) definitions and weights, and the outlier fixed-loss amount. IPPS base rates are updated annually based on the applicable market basket index and estimates of charges in productivity.
For FY 2024, the increase in operating payment rates for general acute care hospitals that are paid under the IPPS, successfully participate in the Hospital Inpatient Quality Reporting (IQR) Program, and are meaningful electronic health record (EHR) users is 3.1%. This reflects a projected FY 2024 IPPS hospital market basket update of 3.3%, reduced by the statutorily required 0.2 percentage point productivity adjustment.
Congress sets the operating rate update by considering the projected increase in the hospital market basket index, which measures the price increases of goods and services hospitals buy to provide patient care.
We pay acute care hospitals an IPPS payment per inpatient case or inpatient discharge.
The admitting hospital, or an entity wholly owned or operated by the admitting hospital, must bill all outpatient diagnostic services and admission-related outpatient non-diagnostic services during the 3 days before admitting the patient to the hospital on the inpatient claim.
Acute care hospitals can’t separately bill Medicare Part B for these services.
Section 1886(d)(1)(B) of the Social Security Act excludes certain hospitals and hospital units from the IPPS. These hospitals and units include:
- Cancer hospitals
- Children’s hospitals
- Extended neoplastic disease care hospitals
- Hospitals located outside the 50 states, the District of Columbia, and Puerto Rico:
- U.S. Virgin Islands
- Guam
- Northern Mariana Islands
- American Samoa
- Inpatient psychiatric facility (IPF) hospitals and units
- Inpatient rehabilitation facility (IRF) hospitals and units
- Long-term care hospitals (LTCHs)
- Religious nonmedical health care institutions (RNHCIs)
Medicare Severity Diagnosis Related Groups
We assign inpatient hospital discharges to MS-DRGs. We use MS-DRGs to better reflect patients’ severity of illness, complexity of service, and hospital resource consumption. An MS-DRG is defined by a group of similar clinical conditions (diagnoses) requiring similar resource use.
The patient’s principal diagnosis, secondary diagnoses, procedures performed, sex, age, and discharge status determine MS-DRG assignment. We consider up to 25 diagnosis and 25 procedure codes for MS-DRG assignment. We review MS-DRG definitions annually to ensure each group has clinically similar conditions that are expected to require similar amounts of inpatient resources.
If our review demonstrates subsets of clinically similar cases within an MS-DRG use significantly different resources, we may propose to reassign them to different MS-DRGs with similar resource use or create new MS-DRGs.
The 3 levels of severity in the MS-DRG system based on secondary diagnosis codes are:
- Major Complication or Comorbidity (MCC) — the highest severity level affecting hospital resource consumption
- Complication or Comorbidity (CC) — the next lowest severity level affecting hospital resource consumption
- Non-Complication or Comorbidity (Non-CC) — the lowest severity level; this level doesn’t significantly affect illness severity and resource use
MS-DRGs may be subdivided (or split) into 2 or 3 severity levels according to these CC subgroups. Some MS-DRGs aren’t subdivided into severity levels, which are known as base MS-DRGs. There are 766 MS-DRGs for FY 2024.
Base Payment Amounts
We set operating and capital IPPS base rates (known as the standardized payment amounts). Operating costs cover labor and supplies, while capital-related costs cover depreciation, interest, rent, and property-related insurance and taxes.
We annually adjust these payment rates for:
- The patient’s clinical condition and related treatment costs compared to average Medicare case costs (MS-DRG relative weight)
- Market conditions in the hospital’s location compared to national conditions (wage index)
Other IPPS Hospital Payments
- Acute care hospitals’ extremely high cost cases can qualify for outlier payments.
- We pay hospitals that train residents in approved graduate medical education (GME) programs separately for the direct cost of training residents (direct GME). We also increase IPPS hospitals’ operating and capital payment rates to reflect teaching hospitals’ higher indirect patient care costs compared to non-teaching hospitals (indirect medical education (IME)).
- For portions of cost reporting periods beginning on or after October 1, 2023, we may consider a rural emergency hospital (REH) to be a nonprovider site and a hospital may include full-time equivalent (FTE) residents training at an REH in its direct GME and IME FTE counts if it meets the nonprovider setting requirements at 42 CFR 412.105(f)(1)(ii)(E) and 413.78(g).
- We increase hospitals’ operating and capital payment rates for treating a disproportionate share of low-income patients. These hospitals also get uncompensated care payments.
- We may also pay acute care hospitals to treat patients with certain newly approved, costly technologies that offer a substantial clinical improvement over existing treatments or that get certain FDA designations for breakthrough devices and antimicrobial products.
- Qualifying rural hospitals and critical access hospitals (CAHs) can get pass-through payments for certain certified registered nurse anesthetist (CRNA) services.
- We pay for the cost of nursing and allied health education activities on a reasonable cost basis subject to conditions and limitations at 42 CFR 413.85(d).
- We pay reasonable and necessary costs for the hospital to get an organ as an adjustment to a hospital’s IPPS payment.
- Hospitals get an add-on payment for the costs of administering blood clotting factors to inpatients with hemophilia.
- We pay an add-on payment to hospitals participating in a National Institutes of Health (NIH)-sponsored islet cell transplantation clinical trial for patients with Type I diabetes.
- We reduce payment in some cases when a patient has a short length of stay (LOS) and transfers to another acute care hospital or, in certain circumstances, to a post-acute care setting.
- IPPS payments are adjusted under the Hospital Value-Based Purchasing (VBP) Program and the Hospital Readmissions Reduction Program (HRRP).
- The Hospital-Acquired Condition (HAC) Reduction Program reduces overall IPPS payments for reasonably preventable HACs.
How We Determine an IPPS Payment
- The hospital submits a claim to its Medicare Administrative Contractor (MAC) for each patient they treat. Based on the claim information, the MAC assigns the case to an MS-DRG.
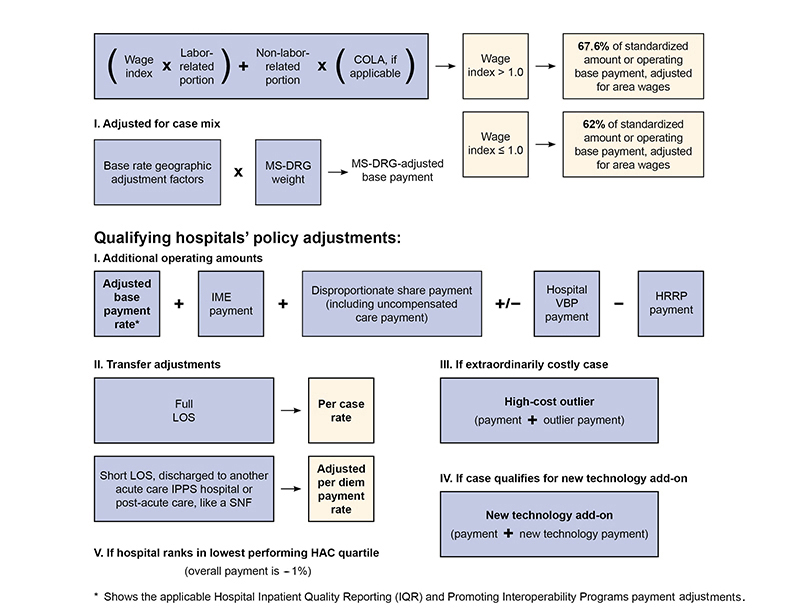
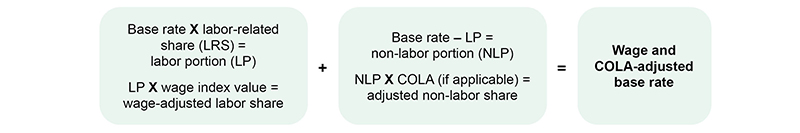
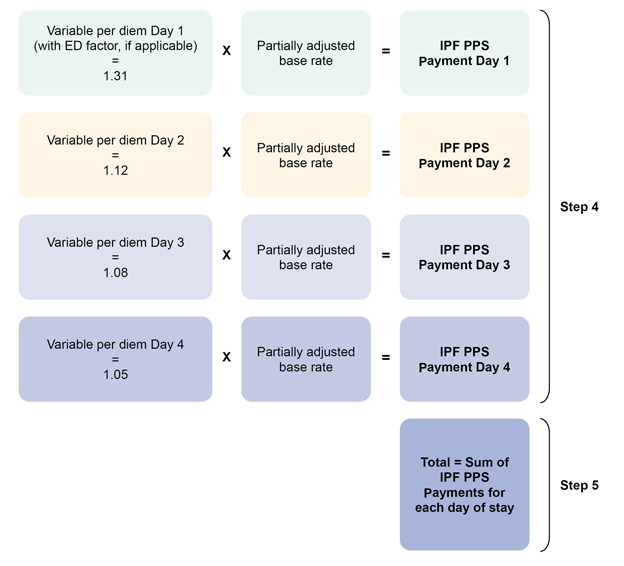
- The base payment rate, or standardized dollar amount, includes the labor-related and non-labor-related share. We adjust the labor-related share by a wage index to reflect area labor cost differences. The labor share equals 67.6% if the hospital’s wage index is greater than 1.0. The law requires that the labor share equals 62% if the hospital’s wage index is less than or equal to 1.0. We adjust the non-labor-related share by a Cost-of-Living Adjustment (COLA) factor equal to 1.0 except for hospitals in Alaska or Hawaii. This adjustment accounts for the higher cost of living in Alaska and Hawaii.
- We multiply the wage-adjusted standardized amount by an MS-DRG weighting factor. The weight is specific to each MS-DRG, and each MS-DRG relative weight represents the average resources to treat cases in that MS-DRG compared to the average resources to treat cases in all MS-DRGs.
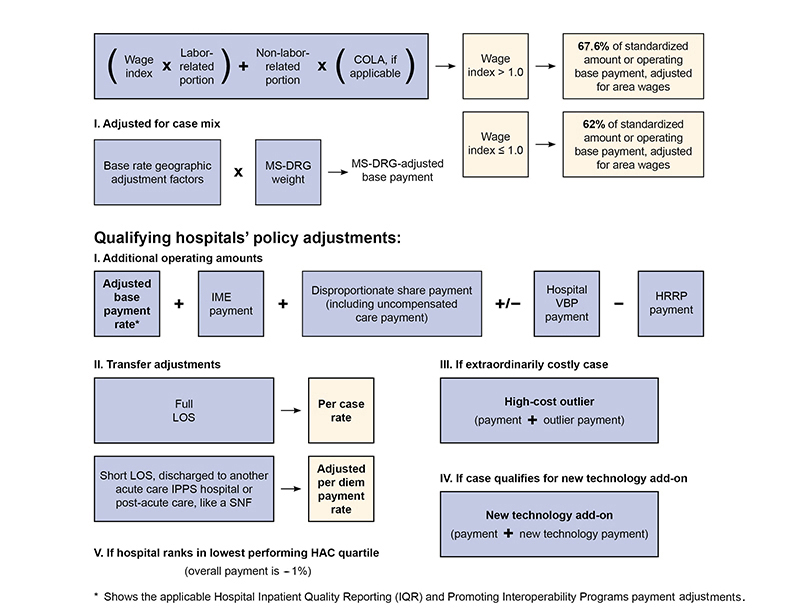
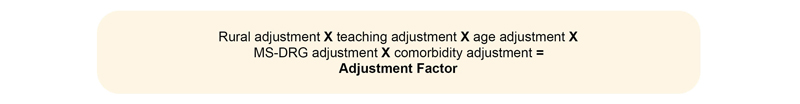
Figure 1. Acute Care Hospital IPPS: Operating Base Payment Rate Adjusted for Geographic Factors
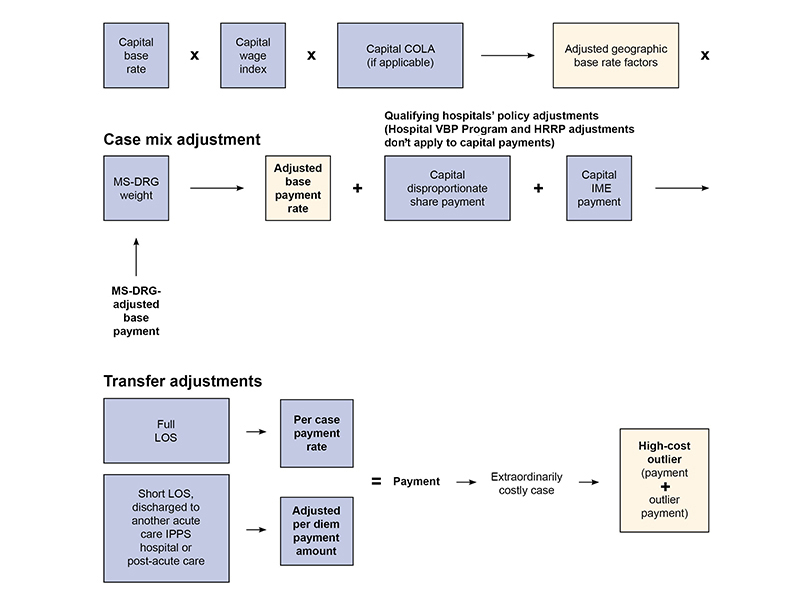
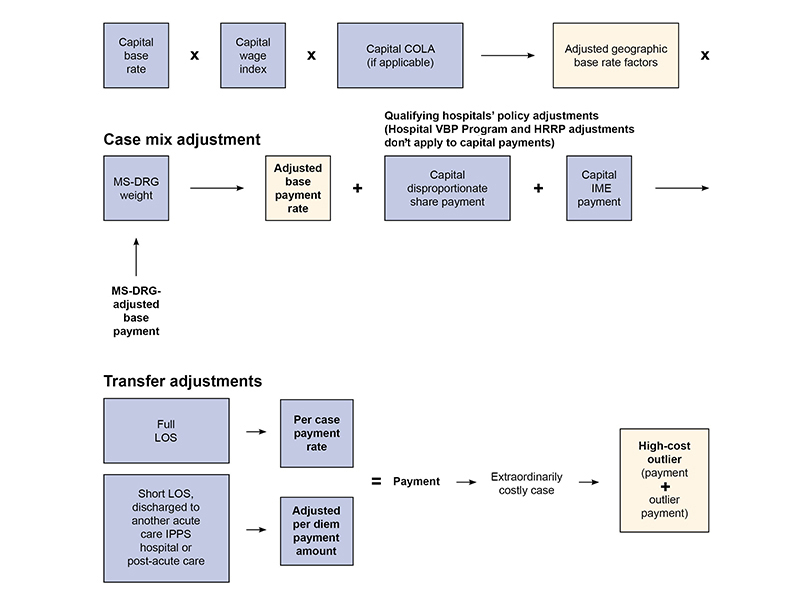
Figure 2. Acute Care Hospital IPPS: Capital Base Payment Rate
MS-DRG Relative Weights
We assign a weight to each MS-DRG that reflects the average case cost in that group compared to the average Medicare case cost and use the same MS-DRG weights for operating and capital payment rates.
We annually adjust the MS-DRG weights without affecting overall IPPS payments, based on standardized charges and all IPPS case costs in each MS-DRG. This adjustment includes a 10% cap on decreases in an MS-DRG relative weight from one FY to another. We standardize hospitals’ billed charges to improve comparability by adjusting:
- Charges to remove differences in hospital wage rates across labor markets
- For the size and intensity of the hospital’s resident training activities
- For the number of low-income hospital patients treated
Note: We reduce charges to costs using national average hospital cost ratios to charges for 19 different hospital departments.
Market Condition Adjustments
We adjust the operating and capital rates by an area wage index to reflect differences in local labor market prices. We measure differences in hospital wage rates among labor markets by comparing the average hourly wage (AHW) for hospital workers in each urban or statewide rural area to the national average.
We use the Office of Management and Budget’s Core-Based Statistical Area delineations, with some modifications, to define each labor market area, and annually revise the wage index based on IPPS hospital wage data.
If a hospital believes it competes for labor in a different area than its location, it may request geographic reclassification through the Medicare Geographic Classification Review Board (MGCRB).
For FY 2024, these policies apply to the wage index:
- We increase the wage index for hospitals with a wage index value below the 25th percentile across all hospitals as we did in FYs 2020 through 2023.
- For FY 2023 and subsequent years, we apply a permanent 5% cap on any decrease to a hospital’s wage index from its wage index in the previous year, regardless of what caused the decline.
- We apply the wage index to the whole capital base rate and raise it to a fractional power, narrowing the geographic variation in wage index values among labor market areas.
- We apply a COLA, reflecting higher supplies and other non-labor resources costs, to the base IPPS operating and capital rates of hospitals in Hawaii and Alaska. We apply the COLA to the non-labor-related portion of the operating base rate and to the whole capital base rate.
Bad Debts
Bad debts are when a patient doesn’t pay their Medicare coinsurance and deductible. We may pay hospital Medicare bad debts at 65% of the allowable amount if they meet all requirements under 42 CFR 413.89.
Providers can collect unpaid patient Medicare cost-sharing amounts, unless the:
- State Medicaid agency classifies the patient as categorically or medically needy
- Provider determines the patient is indigent for bad debt purposes
Providers must submit an acceptable cost report with a detailed bad debt listing corresponding to their claimed bad debt amounts.
Direct Graduate Medical Education
We make direct graduate medical education (DGME) payments to teaching hospitals or hospitals that train residents in approved medical allopathic, osteopathic, dental, or podiatry residency programs. These payments are for the approved residency training programs’ direct operating costs.
We pay these separately from the IPPS per discharge payment and generally base DGME payments on the:
- Hospital-specific costs per resident in a historical base year, updated for inflation
- Number of residents a hospital trains
- Hospital’s Medicare patient load (the proportion of Medicare inpatient days to total inpatient days)
Indirect Medical Education
Teaching hospitals or hospitals that train residents in approved medical allopathic, osteopathic, dental, or podiatry residency programs also get an IME adjustment, which reflects the higher indirect patient care costs of teaching hospitals compared to non-teaching hospitals. We calculate the IME adjustment factor using a hospital’s intern- and resident-to-bed ratio.
Medicare Disproportionate Share Hospitals
We make additional payments for inpatient operating and capital costs to hospitals that serve a disproportionate share of low-income patients.
Hospitals get 25% of the amount they previously got under the traditional Medicare disproportionate share hospital (DSH) statutory formula. The remainder, equal to 75% of what we otherwise would pay as Medicare DSH operating payments, goes toward an uncompensated care payment after reducing the amount for the uninsured individuals’ percentage change.
Each Medicare DSH-eligible hospital gets an uncompensated care payment based on its share of uncompensated care costs compared to all Medicare DSH-eligible hospitals. We annually update the factor estimates that determine each eligible hospital’s uncompensated care payments.
For most DSH-eligible hospitals, we calculate uncompensated care payments from the 2 most recent years of audited Worksheet S-10 data to determine each hospital’s share of uncompensated care payments.
For FY 2024 and subsequent years, we’ll use a 3-year average of the uncompensated care data from the 3 most recent FYs for which audited data is available.
Note: We no longer use low-income insured days as a proxy for uncompensated care to determine Worksheet S-10 Factor 3 for Indian Health Service (IHS), tribal hospitals, and hospitals in Puerto Rico. We’re establishing a new supplemental payment for these hospitals.
Sole Community Hospitals
A Medicare IPPS hospital is eligible for sole community hospital (SCH) classification if it meets 1 of the criteria in 42 CFR 412.92.
We don’t consider a nearby hospital to be a “like hospital” if its total inpatient days attributable to units of the nearby hospital that provides a level of care characteristic of the level of care payable under the acute care hospital IPPS are less than or equal to 8% of similarly calculated total inpatient days of the hospital seeking SCH status.
We base SCH operating payments on the higher of their hospital-specific payment rate or the federal rate and base capital payments on the capital base rate (like all other IPPS hospitals).
SCHs may qualify for a payment adjustment if they experience a significant volume decrease.
For IPPS purposes, we treat certain hospitals formerly designated as essential access community hospitals (EACHs) as SCHs.
Medicare Dependent Hospitals
A Medicare IPPS hospital is eligible for Medicare dependent hospital (MDH) classification if it meets the criteria in 42 CFR 412.108.
We base MDH operating payments on the higher of the federal rate payment or the federal rate payment plus 75% of the difference between the federal rate payment and its hospital-specific rate payment.
Section 4102 of the Consolidated Appropriations Act, 2023, extended the MDH program through September 30, 2024.
Rural Referral Centers
The Rural Referral Center (RRC) Program supports high-volume rural hospitals. We generally classify a Medicare participating acute care hospital as an RRC if it’s in a rural area for IPPS payment purposes and meets the criteria in 42 CFR 412.96.
Current RRCs or hospitals that previously had RRC status get certain advantages:
- Proximity for MGCRB Reclassification: A hospital currently or previously designated as an RRC doesn’t need to demonstrate proximity to the area it gets reclassified. A hospital can apply for reclassification to the closest urban or rural area.
- AHW Data Comparison for MGCRB Reclassification: We exempt hospitals currently or previously designated as the requirement that a hospital’s AHW must exceed, by a certain percentage, the AHW of the labor market area where the hospital is located.
- Medicare DSH Cap: We exempt hospitals designated as an RRC from the 12% cap on Medicare operating DSH payments applicable to other rural hospitals.
Low-Volume Hospitals
Section 4101 of the Consolidated Appropriations Act, 2023, extended the temporary changes to the low-volume hospital payment adjustments through September 30, 2024.
For FYs 2019 through 2024, we make add-on payments to qualifying low-volume hospitals more than 15 road miles from the nearest subsection (d) hospital if it discharges less than 3,800 total patients during the FY based on its most recently submitted cost report:
- Qualifying low-volume hospitals get an additional adjustment of 25% for each Medicare patient discharge
- For low-volume hospitals with 500 or fewer total discharges, the low-volume hospital payment adjustment is 0.25
- For low-volume hospitals with more than 500 total discharges but less than 3,800 total discharges, we calculate the low-volume hospital payment adjustment as 0.25 – [0.25/3300] × (number of total discharges – 500) = (95/330) – (number of total discharges/13,200)
Outlier Payments
We make additional payments for extremely costly outlier cases to promote seriously ill patients’ access to high quality inpatient care. We identify these cases by comparing their estimated operating and capital costs to a fixed-loss threshold.
We annually set the fixed-loss threshold and adjust it to reflect local labor market costs.
We pay outliers by offsetting reductions in the operating and capital base rates (reducing the payment rates to all cases so outlier payments don’t increase or decrease estimated aggregate Medicare spending).
We set the national fixed-loss threshold at 5.1% of total FY payments. For FY 2024, we’ll use the same FY 2020 methodology to incorporate a projection of operating outlier payment reconciliations for the FY 2024 outlier threshold calculation.
Transfer Policy
We reduce MS-DRG payments when the patient’s LOS is at least 1 day less than the geometric mean MS-DRG LOS and 1 of these:
- The hospital transfers the patient to another IPPS-covered acute care hospital or, for certain MS-DRGs, a post-acute care setting
- The hospital transfers the patient to a hospital not participating in Medicare
- The hospital transfers the patient to a CAH
Our transfer policy includes these post-acute care settings:
- Cancer hospitals
- Children’s hospitals
- Home health care, when the patient gets clinically related care beginning within 3 days after a hospital stay
- Hospice care
- LTCHs
- Psychiatric distinct part units located in an acute care hospital or CAHs
- Psychiatric facilities
- Rehabilitation distinct part units located in an acute care hospital or CAHs
- Rehabilitation facilities
- SNFs
New Technology Add-On Payments
We make an additional payment for new medical services and technologies that meet the criteria in 42 CFR 412.87(b).
Certain new transformative devices and antimicrobial products may qualify under an alternative inpatient new technology add-on payment pathway discussed in 42 CFR 412.87(c) and (d).
The Medicare Electronic Application Request Information System™ (MEARIS™) allows users to submit new technology add-on payment applications, requests for ICD-10-PCS procedure codes, or MS-DRG classification change requests. Beginning with FY 2024 MS-DRG classification change requests, we’ll only accept requests submitted through MEARIS and we’ll no longer accept email requests.
Hospital Readmissions Reduction Program
The Hospital Readmissions Reduction Program (HRRP) encourages hospitals to improve communication and care coordination to better engage patients and caregivers in discharge plans and, in turn, reduce avoidable readmissions. The program supports the national goal of improving health care for Americans by linking payment to the quality of hospital care.
Find HRRP data in the provider data catalog. We also adopted MEDPAR data that aligns with the applicable period’s HRRP calculation.
Hospital Value-Based Purchasing Program
The Hospital Value-Based Purchasing (VBP) Program delivers upward, downward, or neutral adjustments to participating hospitals’ base operating MS-DRG payments, based on their quality measure performance. We fund value-based incentive payments by reducing hospitals’ base operating MS-DRG payment amounts. Hospitals may earn back more than, all, or less than the applicable reduced percentage each year. The Hospital VBP Program generally applies to all acute IPPS hospitals, with certain exceptions.
The applicable reduction to hospitals’ base operating MS-DRG payment amount is 2%. Each hospital gets a value-based incentive payment amount that matches their 2% reduction to the base operating MS-DRG payment amount. We’ll continue using the revised scoring and payment methodology adopted in FY 2022 and hospitals won’t get total performance scores (TPSs).
Hospital-Acquired Condition Reduction Program
A hospital-acquired condition (HAC) is a condition a patient gets during hospitalization (the condition wasn’t present on admission). The HAC Reduction Program is a value-based purchasing program that links Medicare payments to health care quality in the inpatient hospital setting.
We reduce overall Medicare IPPS payments (by 1%) for hospitals that rank in the worst-performing quartile of all hospitals on measures of HACs. Under the HAC, hospitals are ranked on their total of preventable conditions, like falls, surgical site infections, and catheter-associated urinary tract infections.
The Hospital Inpatient Quality Reporting Program makes quality of care information available so patients can make informed decisions about their health care options. It also encourages hospitals and providers to improve the quality of inpatient care they provide to patients by ensuring they’re aware of, and reporting on, best practices for their facilities and type of care.
Find current quality reporting measures on the Quality Net website.
Hospitals that don’t report quality data get a 1/4 reduction to the percentage increase in the market basket index. For hospitals that aren’t meaningful EHR users and don’t get an exemption, 3/4 of the percentage increase is further reduced by 100% for FY 2024.