About the Quality Rating System (QRS)
The Quality Rating System (QRS) is a quality reporting program that compares the performance of Qualified Health Plans (QHP) offered on Exchanges and accounts for both the quality of provided healthcare services and the health plan administration. CMS calculates ratings on a 1-to-5 scale (5 is the highest) each year for eligible QHPs in all Exchanges.
The goals of the QRS are to:
- Provide comparable and useful information to consumers about the quality of health care services and enrollee experience with QHPs offered through the Exchanges,
- Facilitate oversight of QHP issuer compliance with quality reporting standards set forth in the Patient Protection and Affordable Care Act and implemented regulations, and
- Provide actionable information that QHP issuers can use to improve quality and performance.
CMS anticipates issuing QRS technical guidance at least annually. CMS also expects to refine the QRS and QHP Enrollee Survey over time based on experience with measuring and reporting quality performance for QHPs offered through the Exchanges. CMS proposes and communicates refinements to the QRS and QHP Enrollee Survey annually through a Call Letter process or the information collection request process per the Paperwork Reduction Act requirements (as appropriate).
Information for Consumers:
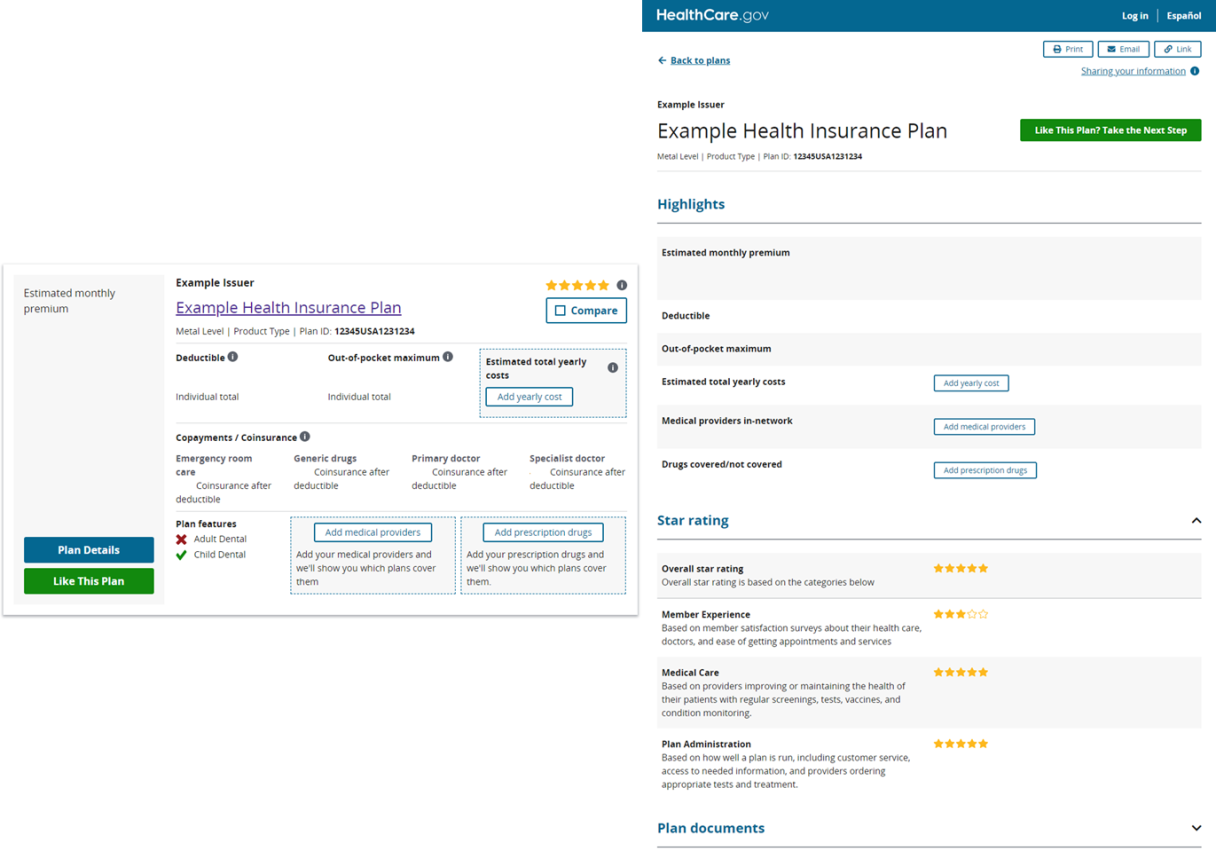
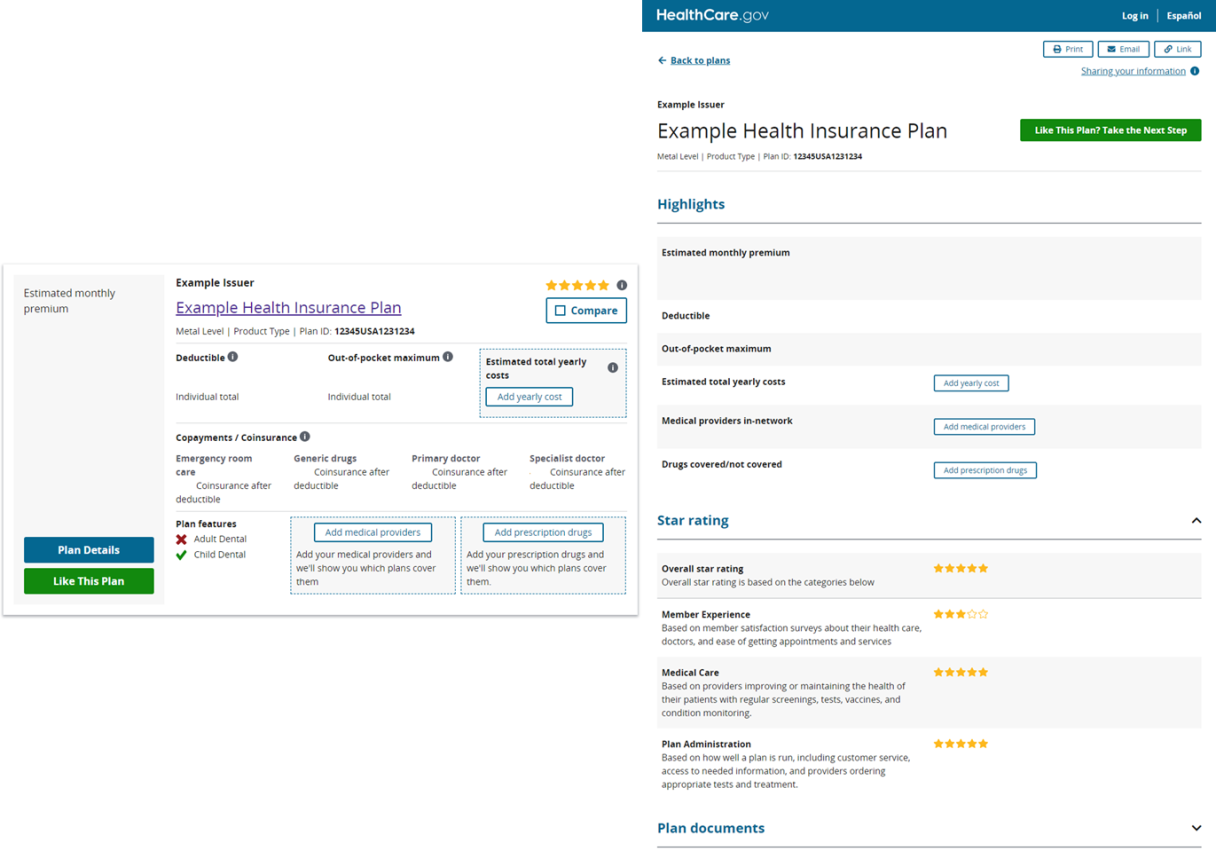
CMS uses a star rating between 1 and 5 (5 is the highest) to demonstrate how a health plan compares to other plans on HealthCare.gov. Health plans receive an Overall Rating which accounts for three categories: Medical Care, Member Experience, and Plan Administration. Multiple measures of quality are considered when rating the plans, broken up into the three categories:
- Medical Care is based on how well the plans’ network providers manage member health care (like Diabetes Care).
- Member Experience is based on surveys of member satisfaction (like Rating of Personal Doctor).
- Plan Administration is based on how well the plan is run (like Access to Information).
Learn more about the quality ratings on HealthCare.gov here: Choosing a High-Quality Marketplace Plan – Last updated September 2022
Background
Section 1311(c)(3) of the Patient Protection and Affordable Care Act (PPACA) directs the U.S. Department of Health & Human Services (HHS) Secretary to develop a system that rates QHPs based on relative quality and price. It also requires Exchanges to display QHP quality ratings on Exchange websites to assist in consumer selection of QHPs. Based on this authority, CMS established standards and requirements related to QHP issuer data collection and public reporting of quality rating information in every Exchange. QHP issuers must submit quality rating information (specifically QRS clinical measure data and QHP Enrollee Survey response data) for its QHPs in accordance with CMS guidelines as a condition of certification and participation in the Exchanges.
CMS aligned federal quality reporting standards for QHP issuers with other federal and state quality reporting program standards, as well as with the Meaningful Measures Initiative. This standardization aims to identify the highest priority areas for quality measurement and quality improvement to assess core quality of care issues that are most vital to advancing the agency’s work to improve patient outcomes.
Quality Rating Display
In 2017, 2018, and 2019, CMS displayed QRS star ratings on HealthCare.gov in select FFE states as part of a limited, phase-in pilot program. Beginning in 2020, CMS displayed quality rating information for all Exchanges that used the HealthCare.gov platform, including the FFEs and SBE-FPs. SBEs that operate their own eligibility and enrollment platform were also required to display quality ratings beginning in 2020 but have some flexibility to customize the display of the QHP quality rating information.
The Quality Rating Information Bulletin announces guidance for public display of quality rating information by all Exchanges, including Federally-facilitated Exchanges (FFE), inclusive of FFE states where the state performs plan management functions, State-based Exchanges on the Federal Platform (SBE-FPs), and State-based Exchanges (SBEs).
For a summary of the quality ratings for Plan Year 2026, see the Health Insurance Exchanges Quality Rating System (QRS) for Plan Year (PY) 2026: Results at a Glance (PDF)
For additional information on the Health Insurance Exchange Quality Rating System, see the Health Insurance Exchange Quality Rating System (QRS) 101 (PDF)
Note: Certain materials provided on this website may be subject to third party copyrights.
Information for Issuers and States:
QHP issuers with questions regarding the QRS or QHP Enrollee Survey should contact the Marketplace Services Desk (MSD) (CMS_FEPS@cms.hhs.gov) and reference the Marketplace Quality Initiatives or “MQI-QRS.”
Guidance for Plan Year 2027 (Ratings Year 2026) and Beyond
- QRS and QHP Enrollee Experience Survey Technical Guidance for 2026 (September 2025) (PDF) : CMS posted the QRS and QHP Enrollee Survey: Technical Guidance for 2026. The Technical Guidance provides QHP issuers certified to offer coverage through the Exchanges in 2026 with the QRS and QHP Enrollee Survey guidance required as a condition of certification.
- 2026 Quality Rating System Measure Technical Specifications (September 2025) (PDF) : CMS has posted an updated version of the 2026 Quality Rating System Measure Technical Specifications, which includes guidance on the finalized data submission requirements for the 2026 QRS measure set. Specifically, CMS added callout boxes summarizing the final decision regarding measures and/or measure rates proposed for addition and those proposed for removal in the Draft 2025 Call Letter and finalized in the Final 2025 Call Letter.
- Final 2025 Call Letter (July 2025) (PDF): CMS has posted the Final 2025 Call Letter for the Quality Rating System and the Qualified Health Plan Enrollee Experience Survey to communicate finalized refinements to the QRS and QHP Enrollee Survey programs for the 2026 ratings year and beyond. This document also summarizes comments received on the Draft 2025 Call Letter.
Plan Year 2026 (Ratings Year 2025) Guidance
- Quality Rating Information Bulletin (April 2025) (PDF): CMS released the Quality Rating Information Bulletin (PDF) to announce guidance for public display of quality rating information by all Exchanges, including the Federally-facilitated Exchanges (FFEs), State-based Exchanges on the Federal Platform (SBE-FPs), and State-based Exchanges (SBEs) that operate their own eligibility and enrollment platform, during the individual market Open Enrollment Period (OEP) for the 2026 Plan Year.
- QRS and QHP Enrollee Experience Survey Technical Guidance for 2025 (September 2024) (PDF): CMS posted the QRS and QHP Enrollee Survey: Technical Guidance for 2025. The Technical Guidance provides QHP issuers certified to offer coverage through the Exchanges in 2025 with the QRS and QHP Enrollee Survey guidance required as a condition of certification.
- 2025 Quality Rating System Measure Technical Specifications (September 2024) (PDF): CMS has posted an updated version of the 2025 Quality Rating System Measure Technical Specifications, which includes guidance on the finalized data submission requirements for the 2025 QRS measure set. Specifically, CMS added callout boxes summarizing the final decision regarding measures and/or measure rates proposed for addition and those proposed for removal in the Draft 2024 Call Letter and finalized in the Final 2024 Call Letter.
User Guides
QHP Issuers and States can preview QRS and QHP Enrollee Survey results in the Marketplace Quality Module (MQM) within CMS' Health Insurance and Oversight System (HIOS). In the MQM, QHP issuers and state representatives can access the following:
- QRS Preview Materials (preview reports and proof sheets)
- QRS QHP List
- Quality Improvement reports detailing QHP Enrollee Survey results
The following document provides instructions for accessing the MQM:
- HIOS MQM Quick Reference Guide (PDF) describes the process that QHP issuers will need to follow to register for EIDM, HIOS and the MQM and to preview their quality ratings information and QHP Enrollee Survey results. This document was last updated December 2020.
Information for Researchers:
Please go to the Downloads page to view available Quality Public Use Files (PUFs)
Marketplace Service Help Desk (MSD)
QHP issuers and Exchanges with questions regarding the QRS should contact the MSD at
CMS_FEPS@cms.hhs.gov or 1-855-CMS-1515 (1-855-267-1515) and reference “Marketplace Quality Initiatives- QRS” or “MQI-QRS”.