Medicare Fee for Service Recovery Audit Program
Do you have questions or concerns about the Recovery Audit Program? Please e-mail us at RAC@cms.hhs.gov. Please Do Not send Personal Health Information to this e-mail address.
The Medicare Fee for Service (FFS) Recovery Audit Program’s mission is to identify and correct Medicare improper payments through the efficient detection and collection of overpayments made on claims of health care services provided to Medicare beneficiaries, and the identification of underpayments to providers so that the CMS can implement actions that will prevent future improper payments in all 50 states.
What does a Recovery Audit Contractor (RAC) do?
The RACs conduct both complex and automated post-payment reviews. Automated reviews occur at the system level while complex reviews require a qualified individual to review the medical record. In order to obtain the medical record and any supporting documentation, the RAC shall issue an Additional Documentation Request (ADR). For more information regarding ADRs, please visit: https://www.cms.gov/research-statistics-data-systems/medicare-fee-service-compliance-programs/medical-review-and-education/additional-documentation-request
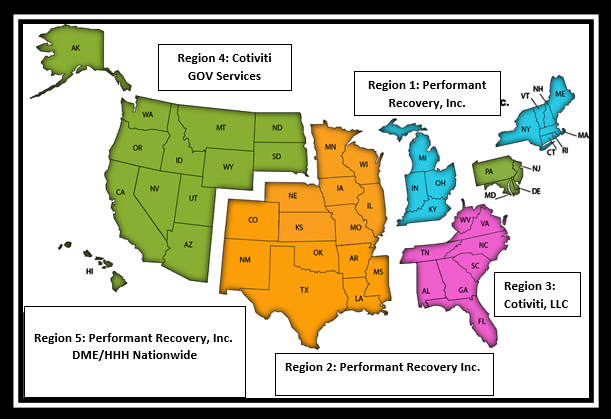
Who are Recovery Audit Contractors?
| Region | States | Websites | Phone Number | |
|---|---|---|---|---|
Region 1 Performant Recovery, Inc. | CT, IN, KY, MA, ME, MI, NH, NY, OH, RI, and VT | info@Performantrac.com | 1-866-201-0580 | |
Region 2 Performant Recovery, Inc. NOTE: Please see March 28, 2023 update below | AR, CO, IA, IL, KS, LA, MO, MN, MS, NE, NM, OK, TX, and WI |
| 1-866-201-0580
| |
Region 3 Cotiviti LLC | AL, FL, GA, NC, SC, TN, VA, WV, Puerto Rico and U.S. Virgin Islands |
| racinfo@cotiviti.com | 1-866-360-2507 |
Region 4 Cotiviti GOV Services (formerly HMS) | AK, AZ, CA, DC, DE, HI, ID, MD, MT, ND, NJ, NV, OR, PA, SD, UT, WA, WY, Guam, American Samoa and Northern Marianas | https://rac4info.cotiviti.com | Part A: 1-877-350-7992 Part B: 1-877-350-7993 | |
Region 5 DME/HHE/Performant Recovery, Inc. | Nationwide for DMEPOS/HHA/Hospice | info@Performantrac.com | 1-866-201-0580 |
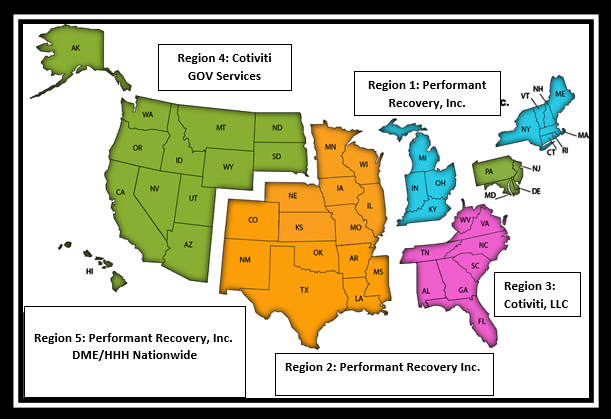
RACs in Regions 1-4 will perform post payment review to identify and correct Medicare claims specific to Part A and Part B.
Region 5 RAC will be dedicated to review of Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) and Home Health / Hospice
What Topics do RACs Review?
Stay in the know on proposed and approved topics that RACs are able to review. These topics will be updated monthly on the RAC reviews topic page and include:
- Name of the Review Topic
- Description of what is being reviewed
- States / MAC regions where reviews will occur
- Review Type (complex review / automated review)
- Provider Types
- Affected Codes
- Applicable Policy References
Recent Updates
March 28, 2023 - On March 24, 2022, CMS awarded Performant Recovery, Inc., the new Recovery Audit Contractor (RAC) Region 2 contract. RAC Region 2 includes the following Medicare Administrative Contractor (MAC) jurisdictions: J5, J6, and JH.
Cotiviti, LLC, the RAC previously responsible for reviews in Region 2, remains under contract with CMS to support the RAC Program from an administrative and appeals perspective in this region. Please contact Cotiviti in regards to reviews conducted by Cotiviti. All notification of improper payments, including review results letters (complex reviews), informational letters (automated reviews) and no findings letters (complex reviews) were completed by Cotiviti, in Region 2, on or before Friday, September 16, 2022.
CMS anticipates Performant will begin reviews in the Spring (2023). RAC Region 2 providers can rely on the review completion date specified in the review results letter, as well as the RAC’s name on the letter, to identify which contractor to reach for inquiries. If Performant receives inquiries in regards to reviews conducted by Cotiviti, Performant customer service will inform providers to reach out to Cotiviti and vice versa.
Region 2 Contact Information:
Cotiviti, LLC
1-866-360-2507
Performant Recovery, Inc.
https://Performantrac.com/providerportal.aspx
1-866-201-0580
March 26, 2021 - CMS awarded Performant Recovery, Inc., the incumbent, the new RAC Region 1 contract.