Pre-Rulemaking
Section 3014 of the Patient Protection and Affordable Care Act of 2010 (ACA) (P.L. 111-148) created section 1890A of the Social Security Act (the Act), which required the U.S. Department of Health and Human Services (HHS) to establish a federal pre-rulemaking process for the selection of quality and efficiency measures for use by HHS. Section 1890(b)(7)(B) of the Act describes the categories of measures.
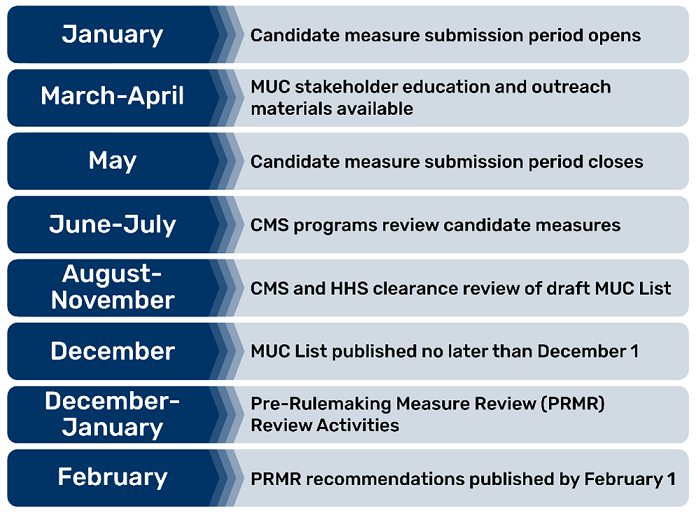
The pre-rulemaking process generally follows these activities:
- Yearly submission of measures by measure developers for CMS consideration through the CMS Measures Under Consideration (MUC) Entry/Review Information Tool (CMS MERIT).
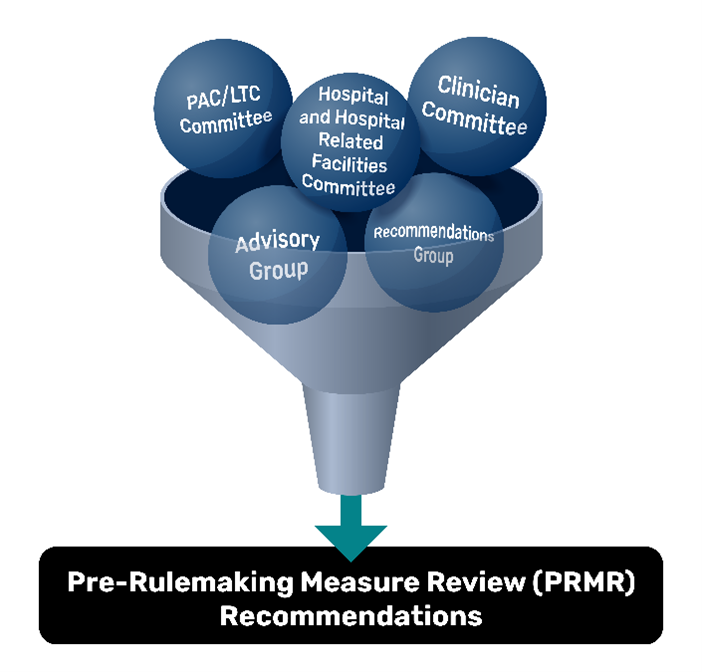
- Publication of a MUC List, no later than December 1st every year, that receives feedback from across HHS, public comment, and diverse groups of interested parties convened by the CMS Consensus-Based Entity.
- Multi-interested party groups provide recommendations to HHS no later than February 1 annually.
- Selected measures enter the federal rulemaking process for additional public comment and consideration before publication of rules finalizing the measures used in CMS programs.
Find pre-rulemaking guidance and resources on the CMS Measures Management System Hub Pre-Rulemaking website.
Contact for More Information
For more information about the pre-rulemaking process, inquiries about measures submitted for consideration, or questions on other general measure topics, please email MMSsupport@battelle.org.