Targeted Probe and Educate
When Medicare Claims are submitted accurately, everyone benefits.
CMS's Targeted Probe and Educate (TPE) program is designed to help providers and suppliers reduce claim denials and appeals through one-on-one help.
The goal: to help you quickly improve. Medicare Administrative Contractors (MACs) work with you, in person, to identify errors and help you correct them. Many common errors are simple – such as a missing physician's signature – and are easily corrected.
Most providers will never need TPE.
TPE is intended to increase accuracy in very specific areas.
MACs use data analysis to identify:
- providers and suppliers who have high claim error rates or unusual billing practices, and
- items and services that have high national error rates and are a financial risk to Medicare.
Providers whose claims are compliant with Medicare policy won't be chosen for TPE.
What are some common claim errors?
How does traditional TPE work?
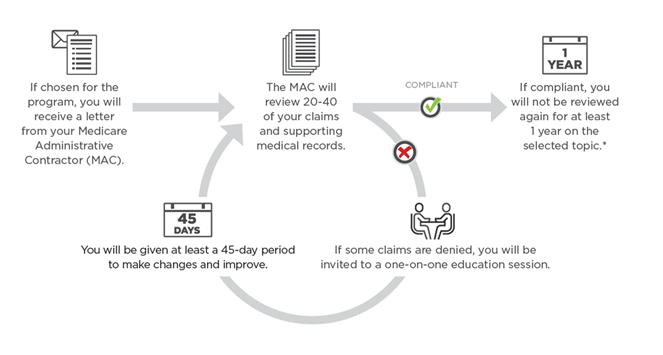
*MACs may conduct additional review if significant changes in provider billing are detected
What if my accuracy still doesn't improve?
This should not be a concern for most providers. The majority that have participated in the TPE process increased the accuracy of their claims. However, any problems that fail to improve after 3 rounds of education sessions will be referred to CMS for next steps. These may include 100 percent prepay review, extrapolation, referral to a Recovery Auditor, or other action.
Is TPE always 20-40 claims in each round?
Generally, a traditional TPE round consists of 20-40 claims but there are variations. For example, CMS has initiated the Low Biller Probe and Educate Program. This nationwide program is designed to include and provide education to providers and suppliers who have lower claim volumes and would otherwise not be selected for the traditional TPE program. Consistent with TPE, MACs will focus on those providers/suppliers who, based on data analysis, provide the most risk to the Medicare program and could benefit from education.
This program focuses on a review of less than 20 claims per round for up to three rounds. Education remains a focus and will be provided after each round.
Learn More About the TPE Program
View, print or share information on the TPE program with this simple one-pager (PDF).
For further details and information about the TPE program, check out this list of TPE Q&As (PDF).
*Note: While TPE is the primary tool used to address errors and provide education to prevent claim denials, CMS also may approve other types of medical reviews in certain circumstances (e.g. service specific medical reviews).