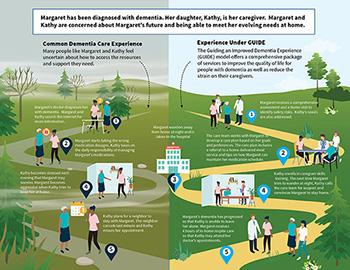
The GUIDE Model provides Medicare coverage for a comprehensive package of care coordination and care management for people with dementia, along with support for qualifying caregivers including education and respite services. The model’s interventions help people with dementia to remain in their homes and communities while supporting caregiver health and wellbeing.
GUIDE Model Dementia Pathways Infographic (PDF)
GUIDE advances key goals of the National Plan to Address Alzheimer’s Disease, which was established through the bipartisan National Alzheimer’s Project Act (NAPA) and has, for over a decade, accelerated federal actions to optimize the quality of care for people with dementia and their caregivers while advancing research towards a cure.
Background
More than 6 million Americans live with dementia with 14 million projected cases by 2060. Despite the disease affecting millions of Americans, many people with dementia do not receive consistent, high-quality coordinated care. This results in poor outcomes, including high rates of hospitalization, emergency department visits, post-acute care utilization, and even death. They also may have high rates of depression, behavioral and psychological symptoms, and poor management of co-occurring conditions.
Dementia care significantly impacts family and unpaid caregivers who provide significant assistance with personal care, financial needs, household tasks, medication management, and clinical coordination. These caregivers commonly report high levels of stress and depression, which negatively affect their health and increase their risks for serious illness, hospitalization, and mortality.
Model Aims
The GUIDE Model aims to:
- Help people with dementia remain safely in their homes longer, delaying facility or long-term nursing home care
- Reduce hospitalization, emergency department use, post-acute care needs, and other costly expenditures
- Address unpaid caregiver needs through improved access to evidence-based education and training, support services and resources, including respite care
- Improve quality of life for people living with dementia by offering comprehensive services and supports through an interdisciplinary care team
- Enhance coordination between interdisciplinary care teams and community-based organizations
Innovation
The GUIDE Model uses an alternative payment methodology to deliver comprehensive, coordinated dementia care. Key innovative payment components include:
- Monthly dementia care management payment – CMS provides tiered monthly per-patient payments to support a collaborative care approach based on patient complexity and caregiver burden, with payments adjusted as a result of participant performance across quality measures.
- Respite services payment – CMS reimburses participants up to $2,500 annually per eligible patient for services that temporarily relieve qualifying caregivers of their caregiving responsibilities, including in-home care, adult day center programs, and facility-based respite.
Design
The GUIDE Model establishes a standardized care delivery approach for dementia care:
- Interdisciplinary care teams – Teams include clinicians with dementia experience, Care Navigators, and direct care workers providing comprehensive, person-centered care.
- Care navigation – Model participants assign aligned Medicare patients with dementia and their caregivers to Care Navigators who facilitate access to clinical services and community-based non-clinical services and resources.
- 24/7 access – Participants provide round-the-clock support lines for urgent questions and concerns.
- Caregiver support – Participants are required to offer caregiver training and support services, as well as connections to community-based providers and resources to reduce caregiver burden based on the caregiver’s needs and responsive to ongoing changes in need.
- Addressing health-related social needs – Participants are required to screen patients and caregivers for psychosocial needs and health-related social needs and connect them with local community-based organizations for comprehensive support to address financial and logistical hurdles such as meals and transportation.
GUIDE also includes a focus on serving people with dementia who are dually eligible for Medicare and Medicaid, with specific components designed to reach high needs populations:
- Financial and technical support for developing dementia care programs in underserved areas, particularly rural communities with limited access to specialty dementia care
- Data-driven targeting of improvement activities
- Financial support to ensure that participating safety-net providers can develop infrastructure and care delivery capabilities for successful model participation